Thrombectomy offers survival benefit for acute stroke
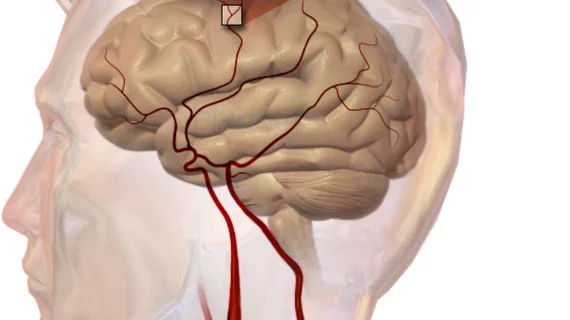
Endovascular thrombectomy (EVT) significantly reduced the risk of 90-day mortality in patients with acute ischemic stroke compared to medical therapy alone, according to a meta-analysis of 10 randomized trials cited in the 2018 update to American stroke guidelines.
The authors drew a parallel from acute ischemic stroke (AIS) care to interventions for acute myocardial infarction. They pointed out that intravenous thrombolysis (IT) was originally offered as a way to improve outcomes in both instances but was later deemed inferior to interventional strategies—primary PCI in the case of acute MI and EVT in the case of AIS.
“However, unlike with the use of IT for myocardial infarction, mortality benefits of IT for AIS were not seen in short-term or long-term follow-up (of randomized trials),” lead author Yingfeng Lin, MD, with Heinrich-Heine-University in Dusseldorf, Germany, and colleagues wrote in JAMA Neurology. “In logic succession, all EVT trials focused on measures of functional recovery from AIS and were underpowered to detect differences in mortality, just like subsequent meta-analyses.”
To better analyze whether thrombectomy also comes with a survival benefit, Lin et al. pooled results from 10 randomized clinical trials of EVT versus medical therapy which were cited in the American Stroke Association/American Heart Association’s 2018 guidelines for AIS.
For the 2,313 patients included in those studies, EVT reduced by 3.7% the odds of 90-day mortality compared to medical therapy (15% vs 18.7%). The researchers calculated that 27 patients would need to be treated with EVT instead of medical therapy to prevent one all-cause death at 90 days.
This difference was deemed statistically significant and was similar to trials evaluating early-window or late-window interventions. Late-window randomized clinical trials (RCTs) included those in which EVT was offered at least six hours after symptom onset.
However, there was no significant difference in the risk for intracranial hemorrhage over 90 days for patients treated with EVT (4.2%) or medical therapy (4%).
“Thus, the observed risk reduction for mortality probably does not originate from differences in adverse effects but from the functional benefits of EVT also translating to improved 90-day survival,” the authors wrote.
“Taken together, there is considerable evidence in guideline-referenced RCTs that EVT significantly benefits survival during the first 90 days after AIS compared with medical therapy alone. We cannot help but see the parallels: endovascular strategies may well turn out to be as successful in AIS as in myocardial infarction.”
According to the researchers, the inclusion of trials with different designs—such as an early versus late intervention window—along with different generations of devices warrants “considerable caution” when interpreting the results.
“However, new EVT trials designed to show mortality differences in AIS might never be performed; thus, a meta-analysis of available data may be the only way to analyze short-term survival,” they wrote.