One-stop CT, MR imaging: Future in diabetic care?
Quantifying body fat and other clinical factors in obese patients with diabetes using CT or magnetic resonance (MR) may help physicians detect and manage comorbidities such as cardiovascular disease, according to a review published in the May issue of Diabetes Technology & Therapeutics. But is that enough to justify “one-stop shop” imaging?
Kavita Garg, MD, of University of Colorado Denver School of Medicine in Aurora, and colleagues wrote that most imaging in this patient population is ordered for events such as complications from infections or surgeries. But noninvasive imaging provides quantitative information and offers a potential option for procedures such as biopsies to diagnose nonalcoholic fatty liver disease, for instance.
The review summarized current evidence about imaging of body fat and nonalcoholic fatty liver disease, but because diabetic patients are at risk of cardiovascular disease and cancer, the authors also investigated the use of imaging to detect those conditions. “There is an emerging role for imaging in early detection of not only structural but also functional abnormalities of the myocardium at a subclinical stage,” they wrote.
Research points to a correlation between body fat in different areas of the body and clinical disease—for instance, pericardial and visceral adiposity and coronary artery disease—but it is not performed routinely in practice.
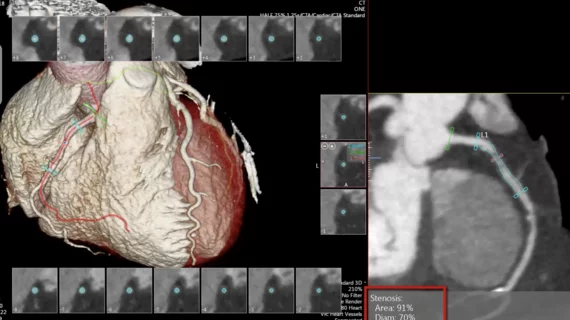
The authors noted that diabetics are more likely than nondiabetics to develop coronary artery calcification. Carotid artery ultrasound, cardiac CT or MR, angiography and intravascular ultrasound have been used to detect lesions. The advantages of cardiac CT include its wide availability and high temporal and spatial resolution, and CT coronary angiography with motion and perfusion analysis provides structural and functional information.
Each modality has drawbacks, from artifacts from prosthetic valves to radiation exposure, although new methods have decreased dose dramatically, they wrote.
Echocardiographic techniques also help detect early-stage disease such as diabetic cardiomyopathy. “At a preclinical stage, echocardiographic techniques such as tissue Doppler imaging and speckle tracking imaging have suggested subclinical systolic myocardial dysfunction in patients with type 2 diabetes,” they wrote. “Such subtle systolic alterations are considered to be early signs of diabetic cardiomyopathy.”
CT or MR may be called for in some circumstances. For instance, obesity poses a problem when using ultrasound for abdominal aortic aneurysm, and CT or MRI may then be indicated. MRI also may be useful for assessing arterial stiffness, which is associated with metabolic syndrome.
Given CT’s capability to quantify body fat, detect cardiovascular disease and cancer and other applications, Garg et al make a case for a “one-stop shop” for imaging obese diabetic patients using a single scan. “Radiologists can now provide information about atherosclerotic and aneurysmal changes of abdominal aorta, body composition, hepatic steatosis, steatohepatitis, cirrhosis, hepatocellular carcinoma, or other cancers such as pancreatic, renal, adrenal, gastric, and colon, from one abdominal CT or MR scan.”
But radiologists should not stop there, the authors wrote. They will need to standardize reports highlighting relevant clinical findings, give follow-up recommendations for managing these patients and recognize that this approach increases costs.
In an accompanying editorial, Viswanathan Mohan, MD, PhD, of the World Health Organization Collaborating Centre for Non-Communicable Diseases Prevention and Control in Gopalapuram, India, described Garg et al as trend setters, but cautioned that clinical trials were needed to prove the efficacy, safety and cost-effectiveness of routine imaging of obese diabetic patients.
“However, at least in high-risk individuals, it is time that we started screening for these conditions because if detected early, the long-term prognosis could be improved,” he wrote.