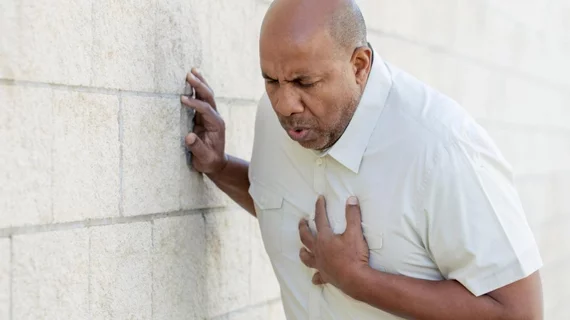
Chill factor: Cardiac-related admissions, mortality increase in the winter months
Two studies suggest patients with cardiac-related hospitalizations—specifically for aortic dissection and ST-segment elevation myocardial infarction (STEMI)—are admitted more frequently and have higher mortality rates during winter months. Results of the studies were presented at the Society for Cardiovascular Angiography and Interventions 2018 Scientific Sessions in San Diego on April 26.
In the first study, researchers estimated the annual number of hospitalizations for aortic dissection over a 12-year period by dividing the number of hospitalizations per month by the number of days per month.
There were 6,199 hospitalizations with a primary diagnosis of aortic dissection, which were further grouped by season. The results showed hospitalizations occurred most often in January and bottomed out in June.
"While earlier studies have shown seasonal variations for other cardiac conditions, this is the first time we found an impressive pattern of seasonal variation in hospitalizations in the U.S. specifically for aortic dissection," said lead researcher Dhara Patel, MD, with the Central Michigan University College of Medicine in Mount Pleasant, Michigan.
Patel added that her group wants to continue researching to understand why more hospitalizations due to aortic dissection occur in the winter.
“It is our hope that by understanding the connection between colder months and aortic dissection, we can ultimately prevent future cases and help improve patient outcomes," Patel said.
The second study assessed the hospital admittance rates more than 827,000 STEMI patients from the Nationwide Inpatient Sample database by weekday, weekend and month during a four-year period. There were 595,452 patients admitted during weekdays and 231,745 during the weekend.
The results showed patients who were admitted with STEMI had a higher mortality rate in winter than summer. There was a 6.1 to 6.7 percent rate of mortality from June to August, whereas December to February saw an increase of 7.2 to 7.6 percent.
“Our study is the largest of its kind to look at the effect of admission day/month on STEMI outcomes, and our results show a higher mortality rate in winter months,” said lead author, Chowdhury Ahsan, MD, at the University of Nevada Las Vegas School of Medicine. “Patients included in this study transferred locations at some point while receiving care, which only stresses the vital importance of having an interconnected healthcare system to decrease mortality rates during winter months and deliver optimum patient care.”