Coronary artery calcium signals greatest mortality risk in blacks, Hispanics
Coronary artery calcium (CAC) is predictive of all-cause and cardiovascular mortality across all racial and ethnic groups, according to a study published in the Journal of the American Heart Association—but the risk of those outcomes is significantly higher across all CAC scores for black and Hispanic patients than for whites and Asians.
This issue has been a topic of debate, noted senior author Michael J. Blaha, MD, MPH, and colleagues, because previous reports gave conflicting evidence on whether CAC scores provided similar prognostic information across racial subgroups. In fact, they wrote, most risk prediction tools have “questionable applicability to ethnic minorities.”
“The Pooled Cohort Equation, for example, only has equations for non‐Hispanic whites and blacks, and in the absence of good evidence, provides a general recommendation for using the non‐Hispanic white equations for all other ethnic groups,” Blaha and coauthors wrote. “These assumptions fail to accurately predict risk in these populations.”
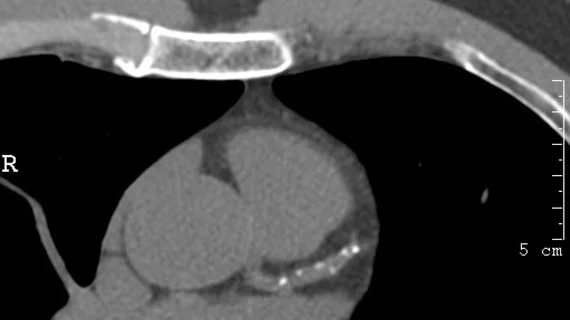
To better understand how CAC scoring applied to each group, the researchers studied 42,224 participants from the CAC Consortium, the largest available cohort of CAC scoring. Participants included 38,277 whites, 1,621 Asians, 1,349 Hispanics and 977 blacks—all of whom had CAC scanning assessed by CT and risk factor and laboratory data collected as part of routine visits to health clinics.
Blacks and Hispanics showed higher risks of cardiovascular mortality during the median 11.7 years of follow-up than whites and Asians, even when CAC scores were zero. Using a statistical model adjusting for traditional risk factors and CAC scoring, blacks showed a 3.4-fold risk of CVD mortality while Hispanics had a 2.3-fold risk compared to whites.
“We think these results are important when viewed through the lens of healthcare disparities in the United States,” Blaha et al. wrote. “Similar to studies that have shown that the Pooled Cohort Equations estimates higher 10‐year ASCVD (atherosclerotic CVD) risk in blacks compared with whites, given the same burden of traditional cardiovascular risk factors, our findings suggest that that blacks and Hispanics have excess CVD mortality over whites and Asians even when they have similar calcified atherosclerotic burden.”
The gradient in increased all-cause mortality risk was also steeper in those ethnic minorities. For example, whites with CAC scores between 100 and 399 had a 1.4-fold risk of all-cause mortality compared to whites with no CAC, while blacks in that same range had triple the risk of all-cause mortality compared to blacks with CAC scores of 0. The difference got even more extreme for CAC scores above 400, which signaled 5.2 times the odds of mortality in blacks but just a 2.2-fold risk of mortality in whites versus people in those groups with no CAC.
The authors also found that adding CAC to the factors included in the Framingham risk score significantly improved the model’s discrimination. Adding CAC bumped the model’s area under the curve (AUC) from 0.814 to 0.819 in whites, 0.790 to 0.819 in Asians, 0.754 to 0.790 in blacks and 0.745 to 0.770 in Hispanics.
“The improvement in risk prediction in minorities is especially important in the light of recent American College of Cardiology/American Heart Association and US Preventive Services Task Force guideline recommendations to utilize cardiovascular risk prediction tools in guiding therapy,” Blaha and colleagues wrote. “Since available risk calculators may not adequately capture risk in minority groups, these results provide data to support specific recommendations for considering selective use of CAC in minorities to improve ASCVD risk estimation.”
The authors noted their analysis didn’t adjust for socioeconomic factors, which may partly explain the prognostic differences of CAC by race.
“These findings therefore highlight the need to pay more attention to comprehensive risk factor modification in high‐risk race/ethnic minorities,” they wrote. “Additionally, a leveling of cardiovascular mortality risk with similar CAC scores across race/ethnicity groups can be viewed as a simple marker of success in leveling disparities in cardiovascular health care.”