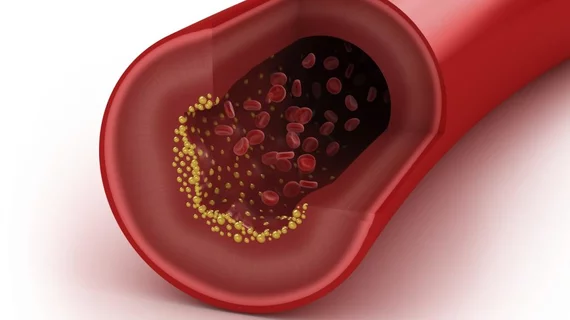
Novel imaging approach tracks atherosclerotic plaque buildup in vivo
Researchers at the University of Tsukuba in Japan have identified a new approach for imaging the progression of atherosclerotic plaque in vivo, according to a study published in Scientific Reports.
The imaging method, developed by authors Yoshihiro Miwa, Michito Hamada and their team at the university, involves expressing a fluorescent protein in immune cells that gravitate to atherosclerotic plaque. The researchers first tested the technique in a group of lab mice, who were exposed to X-rays at the study’s baseline to wipe out their native immune system cells. Those cells were replaced with genetically engineered, fluorescent immune cells.
“A main advantage of our approach is that the introduced immune cells, as macrophages, congregate in atherosclerotic plaque, so the level of fluorescence emitted by them strongly correlates with the amount of plaque that has formed,” Miwa said in a release. “Because the expressed fluorescent proteins emit light in the near-infrared part of the spectrum, they can be detected at deeper locations within the body, such as the thoracic aorta.”
After inactivating a fat and cholesterol-related receptor in the rodents, Miwa et al. induced atherosclerosis in the mice by feeding them a high-cholesterol diet. It was clear the imaging approach worked well to illuminate plaque buildup, but the researchers tested whether they could quantify that plaque by differentiating the animals’ diets. Some continued their high-cholesterol regimen, while others alternated a high-cholesterol and normal diet and a third group ate a normal diet.
Based on the intensity of the fluorescent signal, Miwa and colleagues said they were able to observe stepwise differences in plaque quantity between the three groups. There were also clear increases in buildup the longer a mouse spent consuming an unhealthy diet.
Hamada said in the release the team is looking to increase the sophistication of their novel method, which, when refined, might help scientists track the efficacy of anti-atherosclerotic medications in real time and help analyze CVD risk in individual patients.
“Because we can now clearly analyze the amount of plaque present and its change over time, our work should lead to more effective monitoring of how well anti-atherosclerotic drugs work,” Hamada said. “This method can also reduce the number of experimental animals used because there’s no need to sacrifice them and remove tissues for analysis at each time point within an experiment.”