Researchers question FFR-CT’s value compared to other cardiac imaging options
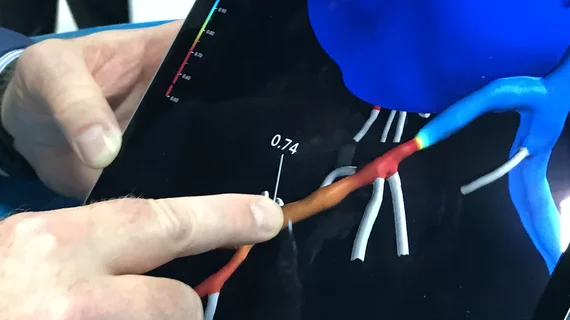
Computed tomography-derived fractional flow reserve (FFR-CT) may have a lower positive predictive value (PPV) than expected, according to a new analysis published in JACC: Cardiovascular Imaging.[1] How could this impact its overall value?
FFR-CT has grown in popularity due its ability to provide noninvasive evaluations of patients being considered for revascularization procedures such as percutaneous coronary intervention. With FFR-CT gaining favor among U.S. and U.K. recommendations—including its place in the 2021 American College of Cardiology/American Heart Association chest pain guidelines—the study’s authors hoped to learn more about its effectiveness from both a clinical and financial perspective.
Lead author Tarun K. Mittal, MD, MSc, an honorary clinical senior lecturer with the National Heart & Lung Institute at Imperial College London, and colleagues examined real-world data from more than 2,200 coronary CT angiograms (CCTAs) that underwent an FFR-CT analysis at one of 12 U.K. facilities. The mean patient age was 61.4 years old, 62.4% of patients were men and the most common indications for the original CCTA were stable chest pain (77.4%), acute chest pain (5.9%) and shortness of breath (5.2%).
Overall, FFR-CT was found to have a PPV of 49% and negative predictive value (NPV) of 76%. Mittal et al. noted that these numbers are lower than the PPV of 65% and NPV of 93% achieved in multicenter trials used to help FFR-CT receive a recommendation from the National Institute for Health and Care Excellence (NICE) back in 2017.
The study’s authors also performed a separate cost analysis of using FFR-CT “as a functional assessment in our practice.” Using pricing data from the U.K., they found that an FFR-CT strategy was associated with an average cost of £2,102 ($2,657) per patient and a stress imaging strategy was associated with an average cost of £1,411 ($1,785). This was mostly due to the “higher rate of invasive coronary angiography (ICA) and revascularization procedures” see with the FFR-CT strategy.
“The results of our real-world audit suggest that FFR-CT in patients with stable chest pain may not be as accurate or cost effective as has been suggested when compared to alternative stress imaging strategies,” the authors wrote. “Although recommended by the guidelines, its widespread use should be undertaken with caution.”
The group also emphasized that additional real-world studies are needed to take a closer look at the potential value of adopting FFR-CT.
Limitations of the FFR-CT study to consider
The study did have several limitations. For example, “as with any observational diagnostic study,” the authors warned that there is always a risk of referral or verification bias.
In addition, the cost analysis was focused on policies in the U.K. and may not necessarily be relevant to U.S. health systems.
“Furthermore, although our study based the pricing of the FFR-CT pathway on our own real-world data, the assumptions and parameters used for stress imaging tests were derived from other studies,” the authors added. “Although they reflect real-world practice, the actual data may vary among institutions.”
Read the full analysis here.