How engineering could optimize the artificial heart valve
Redesigning the artificial heart valve could improve blood flow and potentially eliminate the need for blood thinners in patients with mechanical support, according to a new study.
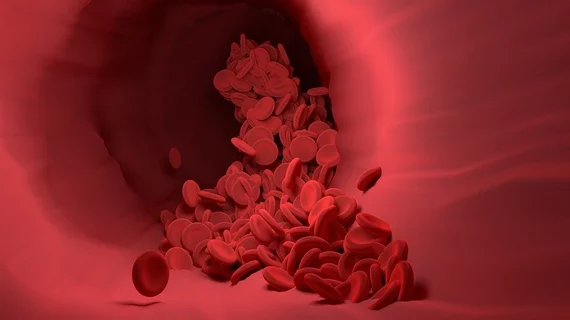
Turbulence in blood vessels—disruptions to blood flow velocity that occur when blood struggles to flow cleanly along vessel bends or edges—is a known risk for blood clots and, if left unaddressed, stroke. That risk is only upped when patients have artificial heart valves, which are known to produce even more turbulent blood flows.
First author Hadi Zolfaghari and colleagues wrote in Physical Review Fluids that scientists are still unsure of why mechanical valves are so much more prone to clot formation than biological heart valves, but artificial valves are a reality for scores of heart patients. Using the complex mathematics of hydrodynamic stability theory, Zolfaghari and his team at the ARTORG Center for Biomedical Engineering Research at the University of Bern set out to design mechanical valves that would optimize flow velocity and reduce any risky turbulence. They said it’s the first translation of these engineering methods, which are used more commonly for aircraft design, into medicine.
The researchers employed advanced computer simulations to identify at least one culprit behind strong turbulence in people with artificial valves: the current shape of flow-regulating heart valve flaps. In a release, Zolfaghari said he and his colleagues were able to discern how blood impinges at the front edge of valve flaps, quickly rendering blood flow unstable.
“The strong forces generated in this process could activate the blood coagulation and cause clots to form immediately behind the valve,” he said. “Supercomputers helped us to capture one root cause of turbulence in these valves, and hydrodynamic stability theory helped us to find an engineering fix for it.”
That fix would include minor structural changes to the mechanical valves used in the study, which were outfitted with a metal ring and two flaps that rotate on hinges. The flaps open and close with each heartbeat to allow blood to flow out of the heart while preventing any backflow, and Zolfaghari et al. said that even slightly modifying the design of the valve flaps allowed blood to flow through the flaps without generating instabilities that could lead to healthy turbulence.
The authors said that if the design of mechanical heart valves is improved from a fluid mechanics point of view, it’s possible that future heart patients with artificial valves might no longer need blood thinners. The more than 10,000 people who receive a mechanical heart valve each year take blood thinners every day for their entire lives, so eliminating the need for those drugs could cut medical costs and complications.
“The design of mechanical heart valves has hardly been adapted since their development in the 1970s,” Dominik Obrist, head of the research group at the ARTORG Center, said in the release. “By contrast, a lot of research and development has been conducted in other engineering areas, such as aircraft design. Considering how many people have an artificial heart valve, it is time to talk about design optimizations also in this area in order to give these people a better life.”