Blood transfusion during surgery boosts risk of venous thromboembolism
Red blood cell (RBC) transfusions during surgery are associated with double the risk of venous thromboembolism (VTE) over the ensuing 30 days, researchers reported in JAMA Surgery.
Investigators analyzed more than 750,000 patients undergoing surgery from a registry containing 525 North American hospitals. A total of 6.3 percent of the patients received perioperative RBC transfusions, defined as a transfusion from 72 hours before to 72 hours after surgery.
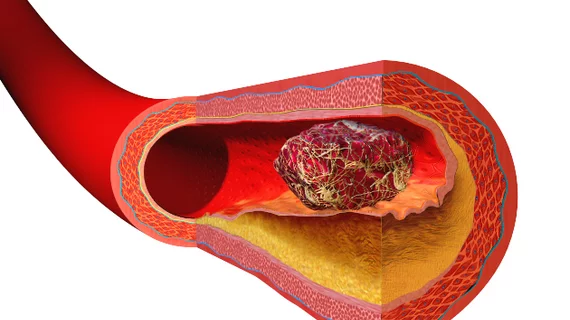
These patients experienced VTE at a rate 2.1 times higher than those who didn’t undergo transfusions, even after adjustment for patient characteristics, surgical complexity and hospital length of stay. However, only 0.8 percent of patients in the study experienced postoperative VTE, a combination of pulmonary embolism and deep vein thrombosis.
“Transfused RBCs have been proposed to modulate the inflammatory cascade,” wrote lead author Ruchika Goel, MD, MPH, with New York Presbyterian Hospital and Weill Cornell Medicine, and colleagues. “In addition, during the storage period, RBCs develop storage lesions, including metabolic, biochemical, and physical changes responsible for accumulation of bioreactive substances such as microparticles, which can have a prothrombogenic potential.
“Because inflammation and hypercoagulation are closely linked, the proinflammatory and immunomodulatory properties of RBC transfusion may further potentiate a hypercoagulable state.”
When analyzing the components of VTE separately, the researchers found RBC transfusions upped the risk of deep vein thrombosis and pulmonary embolism by 2.2-fold and 1.9-fold, respectively.
Goel et al. also conducted a propensity-score matched analysis of 47,142 people who received transfusions against the same number of matched controls who didn’t receive transfusions. Even with this technique to balance patient characteristics, postoperative VTE was 1.9 times more likely to occur in individuals who received transfusions.
“Surgery is a well-recognized prothrombotic stimulus, and in a subset of patients receiving perioperative RBC transfusions, a synergistic and incremental dose-related risk for VTE development may exist,” the authors wrote. “These results need prospective validation in cohort studies and randomized clinical trials; if proven, they underscore the continued need for more stringent and optimal perioperative blood management practices in addition to rigorous VTE prophylaxis in patients undergoing surgery.”