‘Heart-on-a-chip’ system replicates human drug response
TARA Biosystems’ “heart-on-a-chip” system successfully replicates human drug responses to CV medications without having to risk cardiotoxicity in human testing, researchers from TARA and GlaxoSmithKline (GSK) announced August 6.
Cardiac toxicity is responsible for nearly half of new medicine recalls, Nicole T. Feric and colleagues wrote in Toxicological Sciences, but historically there hasn’t been an optimal way to test that kind of toxicity before human use. In vitro systems and animal models don’t fully capture the physiology of the human heart, and more recent attempts to bridge the gap with human induced pluripotent stem cells (hiPSCs) have been met with some difficulty.
“The recent development of robust cardiac differentiation protocols for hiPSCs have provided the potential for an unlimited supply of human-derived cardiac cells from both healthy and diseased sources, but this potential has been limited by the observation that hiPSC-derived cardiomyocytes typically retain a more fetal-like phenotype,” Feric et al. said in the journal. “This raises concerns about the predictability and translatability of results obtained in vitro to the settings of drug safety, discovery and development.”
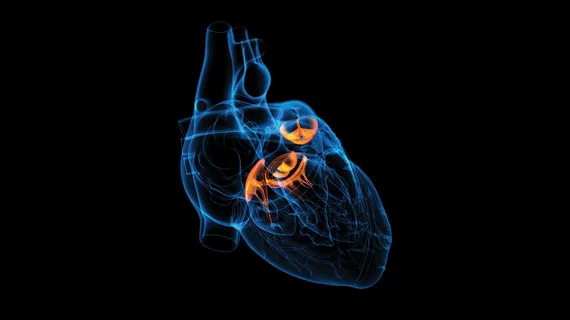
TARA’s platform attempts to mitigate those concerns by subjecting hiPSCs to a rigorous maturation process in its Biowire II system, which is able to render 3D human cardiac tissue (trademarked as “Cardiotype” tissue) from the original hiPSCs. Unlike models that rely on hiPSCs alone, Feric and her colleagues can measure the force with which Cardiotype tissues contract, better reflecting human physiology.
In their latest work, Feric et al. teamed up with researchers from GSK to screen a handful of clinically relevant drugs using the Cardiotype platform. The drugs, all of which had known efficacy and toxicity profiles in the heart, were hand-picked to assess the predictivity of the Cardiotype assay in comparison to contemporary drug screening methods.
The authors said their engineered tissue responded to the range of cardiotherapeutic and cardiotoxic drugs “as expected,” replicating a human-like response that other labs haven’t been able to capture. They even said their heart-on-a-chip responded to the drugs via the same molecular pathways seen in human heart tissue.
“Human engineered cardiac tissues created in the Biowire II platform have adult-like canonical responses to compounds known to affect contractility via an array of physiologically relevant pathways,” Feric and co-authors wrote. “These studies can be conducted under external stimulation, providing investigators with a high degree of experimental control, and with the ability to assess compounds using a non-destructive measurement of contractility early in the drug discovery and development process.”
The team said their platform could also be used to model different heart diseases by extracting hiPSCs from individual patients.
“These results suggest the utility of the Biowire II platform to create disease models via the use of patient-derived hiPSC cardiomyocytes,” they said.