Watchman implantation in AFib patients cost-effective for recurrent stroke prevention
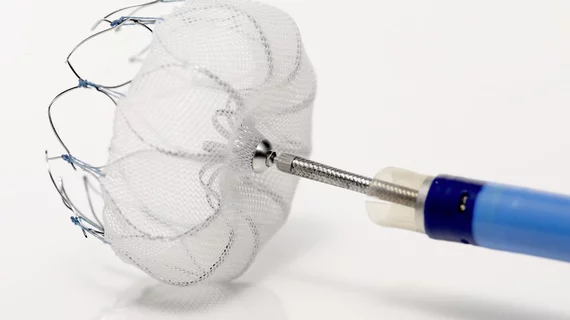
Occluding the left atrial appendage with the Watchman device proved to be a cost-effective strategy for the secondary prevention of stroke among patients with atrial fibrillation (AFib), according to an analysis published in Stroke.
Lead author Vivek Y. Reddy, MD, and colleagues compared left atrial appendage closure (LAAC) with the Boston Scientific device to warfarin as well as the non-vitamin K antagonist oral anticoagulants (NOACs) dabigatran, apixaban and rivaroxaban. From a U.S. Medicare perspective, they analyzed costs for each treatment strategy as well as downstream clinical events including ischemic stroke, transient ischemic attack (TIA), systemic embolism, hemorrhagic stroke, major bleeding and myocardial infarction.
These data were pulled from previous studies evaluating the treatments and extrapolated to 10-year and 20-year outcomes for cost-effectiveness analyses, with 20 years representing the lifetime analysis.
LAAC closure was found to achieve cost-effectiveness at five years relative to dabigatran and at six years relative to warfarin and apixaban, using a willingness-to-pay threshold of $50,000 per quality-adjusted life year (QALY). At 10 years, the operation was associated with at least 0.1 QALY over all of the other treatment options and between $11,154 and $16,039 in savings. Warfarin had the least QALYs gained but also the lowest costs due to its lower price point.
“Upfront procedure costs initially make LAAC higher cost than warfarin and the non–vitamin K antagonist oral anticoagulants, but within 10 years, LAAC delivers more quality-adjusted life years and has lower total costs, making LAAC the most cost-effective treatment strategy for secondary prevention of stroke in atrial fibrillation,” Reddy and colleagues wrote.
The authors noted LAAC was cost-effective in 99.7 percent of simulations, including 100 percent relative to warfarin. It was cost-effective in 90.4 percent of simulations against dabigatran and 95 percent of them against apixaban. Given rivaroxaban was the most expensive of the NOACs and associated with the fewest QALYs, they didn’t run a sensitivity analysis of LAAC versus that particular drug.
Another benefit of LACC is it doesn’t rely on patient adherence the same way medications do, Reddy et al. pointed out.
“Percutaneous LAAC represents a major change in the management of patients with prior stroke or TIA,” the researchers wrote. “It has the inherent benefit of maintaining stroke protection over time without the issue of patient compliance, an important clinical consideration in patients at the highest risk of stroke. These findings should be taken into consideration when formulating policy and practice guidelines for secondary stroke prevention in nonvalvular (AFib).”
The authors acknowledged the body of evidence regarding these secondary stroke preventions in the setting of AFib is “limited,” and noted they had to extrapolate results from the available research out to 10 or 20 years for their analysis. Some of the studies only had about a two-year follow-up, they said.