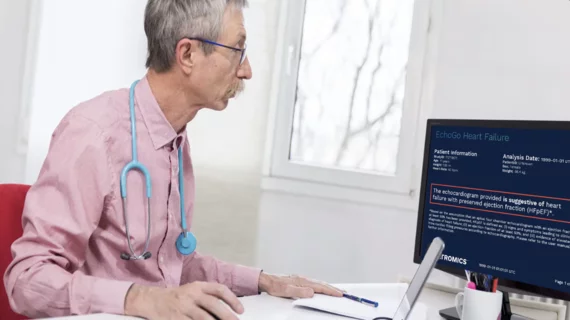
When the Centers for Medicare and Medicaid Services (CMS) finalized the 2024 Hospital Outpatient Prospective Payment System final rule, it included an updated reimbursement for the EchoGo Heart Failure platform from Ultromics.
EchoGo Heart Failure is now associated with an ambulatory payment classification (APC) code of APC 5743 and a payment rate of $284.88. The new rate, up significantly from the prior rate of $99.81, goes into effect on Jan. 1, 2024.
The platform was originally going to be associated with APC 5742 in 2024, but Ultromics relayed to CMS that APC 5743 was more accurate due to the costs incurred by hospitals after the platform has been used for treatment. CMS agreed with this suggestion, as indicated in this update.
“This milestone significantly empowers hospitals to accelerate the integration of EchoGo Heart Failure into their workflow, ultimately improving heart failure with preserved ejection fraction (HFpEF) detection within their healthcare systems,” Ross Upton, PhD, CEO and founder of Ultromics, said in a statement. “Given the prevalence of HFpEF, this development marks a crucial step toward identifying and treating this underdiagnosed condition.”
Additional context about Ultromics and the EchoGo Heart Failure platform
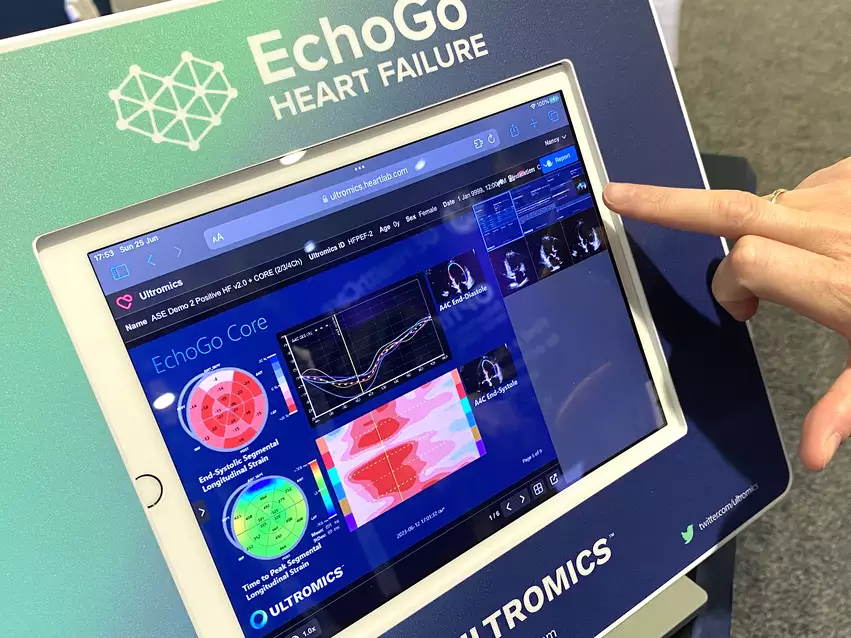
Ultromics is a U.K.-based healthcare technology company focused on heart failure detection. EchoGo Heart Failure, its flagship product, first gained U.S. Food and Drug Administration approval in December 2022. The platform uses advanced artificial intelligence algorithms to detect signs of HFpEF in echocardiogram results.
Ultromics worked closely with Mayo Clinic on the design and development of EchoGo Heart Failure.
“This novel solution applies AI to cardiovascular imaging to greatly simplify identification of patients with HFpEF, a diagnosis that can be challenging to make, and allow more expeditious treatment. HFpEF currently is associated with high rates of hospitalization and mortality,” Patricia A. Pellikka, MD, vice chair of the department of cardiovascular medicine at Mayo Clinic, said when the company’s received FDA approval. “By facilitating early diagnosis and treatment, we can improve the lives of many.”