Revascularization achieved in 83% of distal thrombectomies
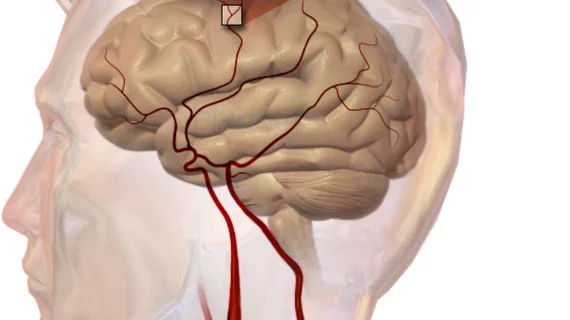
Endovascular therapy (ET) is part of routine care for treating large-vessel occlusion strokes, but the technique is less examined in the setting of distal intracranial occlusions. In a recent study published in Stroke, researchers from Emory University and Grady Memorial Hospital in Atlanta made the case that distal thrombectomy can be safely and effectively utilized in select patients.
Jonathan A. Grossberg, MD, and colleagues studied 69 patients—57 percent male; average age 66.7— who were treated with distal thrombectomy at their hospital between September 2010 and December 2015. Distal occlusion was defined as any segment of the anterior cerebral artery (ACA) or posterior cerebral artery, or occlusion at or distal to the MCA-M3 opercular segment.
Near or complete revascularization was achieved in 83 percent of cases, while 7 percent of patients experienced parenchymal hematomas (PHs). However, only three PHs (4 percent) occurred in the treated territory.
At 90 days, only 30 percent of patients had a modified Rankin Scale score of 0 to 2, consistent with zero to mild disability. Twenty percent of patients died by that three-month mark.
Notably, the median preprocedure National Institutes of Health Stroke Scale Score was 18. The authors said this is higher than what would normally be expected for distal occlusions, acknowledging there may have been selection bias as less severe occlusions would be more likely to be treated with medication alone.
“The 90-day functional outcomes in this study were considerably worse than expected from a series of distal occlusions, which speaks not only to the potential gravity of some of these occlusions, but also calls for further regimented study of these patients,” the authors noted.
The distal occlusion was the primary treatment target for 45 patients in the study, while 23 had the distal occlusion treated as a rescue strategy after a large vessel occlusion stroke. One patient had both primary and rescue treatment.
“Our series demonstrates that these distal thrombectomies are safe to perform,” Grossberg et al. wrote. “Our 7 percent rate of PH is within the 2 percent to eight percent range of symptomatic hemorrhage in the landmark thrombectomy clinical trials. Although this may be high in comparison to what would be expected for simple distal occlusions, the findings should be analyzed in the context of our treated population given their high initial clinical severity and case complexity often involving initially proximal or multiple occlusions.”
The authors acknowledged treating distal arteries is more challenging and risky given their smaller caliber, thinner walls and more “tortuous” nature—especially in the distal superior region, where thrombolytics are preferred. And considering they supply a smaller territory of the brain, the benefit of mechanical treatment may be lessened.
Even so, they said endovascular therapy in these cases is sometimes justified and is now made feasible by technological advances such as smaller stent retrievers.
“We consider that ET in the distal vascular bed represents a very reasonable option for territories of high eloquence, in particular, if there is evidence of a significantly disabling clinical deficit, poor angiographic collateral flow, or there is absence of recovery on the intraprocedural neurological examination after proximal reperfusion alone,” the researchers wrote.
The authors of an accompanying editorial pointed out reperfusions rate were highest (92 percent) when stent retrievers were used. They echoed the investigators’ sentiment that the risk-benefit calculation should weigh that distal arteries supply less brain tissue and would therefore lead to less of a neurological deficit than more severe strokes.
Given this smaller treatment effect, they pointed out a larger sample size would be needed to detect differences in outcomes in a randomized trial, which might not be feasible for this clinical dilemma.
“Other options include matched comparisons of multiple large registry data,” wrote Wolfgang G. Kunz, MD, Mohammed A. Almekhlafi, MD, and Mayank Goyal, MD. “We will have to use our best clinical judgment with extrapolation of everything we learned on (endovascular thrombectomy) and on (intravenous thrombolysis) and be humble in recognizing the limitations of current technology and individual procedural skills.”