IVL vs. RA for chronic total occlusion PCI: Key data cardiologists should know
Intravascular lithotripsy (IVL) and rotational atherectomy (RA) are associated with comparable outcomes when patients undergo chronic total occlusion (CTO) percutaneous coronary intervention (PCI) procedures, according to new research published in The American Journal of Cardiology.[1] However, the study’s authors did still identify a few noteworthy differences.
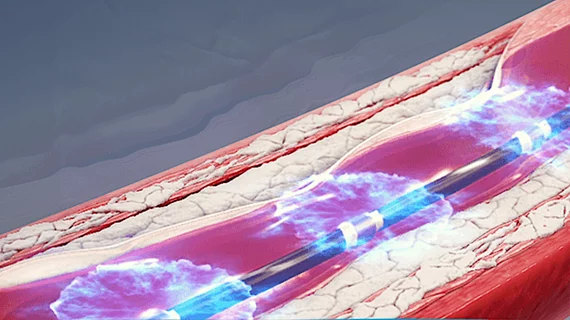
CTO PCI is an interventional procedure reserved for completely occluded coronary arteries. Utilization is expected to grow in the years ahead due to an aging general population, and researchers are still evaluating potential treatment options. IVL is a relatively new technology that was first developed by Shockwave Medical, now a Johnson & Johnson MedTech company, in 2009. RA, meanwhile, has been used to remove plaque buildup for decades and is now more frequently deployed for CTO PCI.
For this latest analysis, researchers tracked data from the PROGRESS-CTO registry. The group identified more than 15,000 CTO PCI patients treated from 2019 to 2024. While 2.8% of those patients were treated with IVL, 2.5% were treated with RA. The mean patient age for both groups was approximately 69 years old. IVL patients tended to have a higher body mass index, were more likely to have a history of prior PCI and were more likely to present with a lower left ventricular ejection fraction. IVL was also more commonly used when CTO lesions were especially complex.
Technical success—defined as successful CTO revascularization with less than 30% residual diameter stenosis in the treated segment and restored coronary blood flow as graded by Thrombolysis in Myocardial Infarction scores—was seen in 97.2% of IVL patients and 95.3% of RA patients. Procedural success—defined as achieving technical success without any major adverse cardiac events—was seen in 94.68% of IVL patients and 91.84% of RA patients. While IVL technically had higher technical and procedural success rates, the differences were not statistically significant.
One significant takeaway from this analysis was the fact that RA was associated with a much higher risk of coronary perforation (9.5%) than IVL (3.2%). A majority, but not all, of the identified perforations occurred in the CTO target vessel.
“Given the lower perforation rate with IVL in our study, IVL may be safer than RA for lesion preparation, and is associated with similar technical and procedural success,” wrote first author Pedro E.P. Carvalho, MD, a cardiologist with the Minneapolis Heart Institute and Minneapolis Heart Institute Foundation, and colleagues.
Diving deeper into the data, Carvalho et al. found a few reasons care teams may want to turn to IVL before RA for their next CTO PCI procedure.
“IVL was utilized in CTO lesions with more complex angiographic characteristics,” they wrote. “Despite this, RA was associated with longer procedural and fluoroscopic times, and radiation doses and contrast volumes were lower in the IVL cohort, suggesting that IVL can streamline and improve procedural workflow and effectiveness of CTO PCI.”
Click here to read the team’s full analysis.