TCT.18: COAPT draws superlatives, raises questions about replicating MitraClip’s benefits
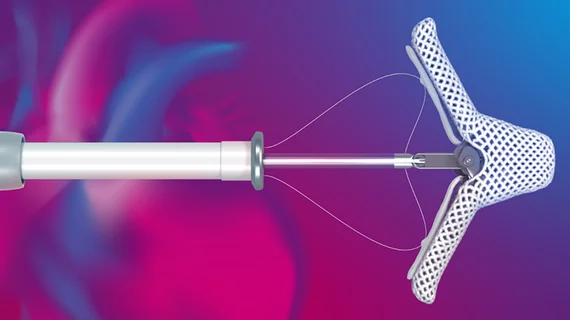
The results of the COAPT trial dropped like a thunderclap Sunday at the Transcatheter Cardiovascular Therapeutics (TCT) annual meeting, with several cardiologists predicting the MitraClip device will have a swift and lasting impact on the treatment of heart failure patients.
Compared to heart failure patients with severe secondary MR who were treated with guideline-directed medical therapy alone, those randomized to the percutaneous clip procedure plus optimal medical therapy demonstrated relative reductions of 47 percent for heart failure hospitalizations and 38 percent for mortality at two years of follow-up. The number of patients required to be treated with Abbott’s MitraClip device to prevent one heart failure hospitalization was three and the number needed to prevent one death at 24 months was six, reported lead investigator Gregg W. Stone, MD, with New York-Presbyterian Hospital and Columbia University Medical Center.
“It just knocks you off your chair how positive this is,” said Jeffrey Popma, MD, with Beth Israel Deaconess Medical Center in Boston.
“I would say this is seminal in this field,” said Michael J. Mack, MD, the medical director of cardiovascular surgery at the Heart Hospital Baylor in Plano, Texas, and co-principal investigator of the study.
“This is really a blockbuster trial,” said Martin B. Leon, MD, also with New York-Presbyterian/Columbia University Medical Center. “It’s a blockbuster trial because you see a statistically significant reduction in cardiovascular mortality, which is something that you almost never see in device-based cardiovascular trials. … You hit your primary endpoint with a number needed to treat of less than 10, in the low single digits, so from that standpoint I think this is a landmark trial that’s going to change clinical practice.”
Superlatives aside, the trial raises important questions about patient selection for the procedure, whether the results are generalizable to routine practice and whether the study can shed more light on the pathophysiology of heart failure.
The trial, published concurrently in the New England Journal of Medicine, randomized 302 patients to the device group and 312 to the control arm of medical therapy alone. The rate of hospitalizations for heart failure—the primary endpoint—was 67.9 percent per patient-year in the control arm and 35.8 percent per patient-year in the device arm. Two-year mortality rates were 46.1 percent and 29.1 percent, respectively.
MitraClip treatment was also associated with improvements across 10 secondary endpoints, including quality-of-life measures, all-cause hospitalizations and severity of mitral regurgitation.
“In patients with heart failure and moderate-to-severe or severe secondary MR who remain symptomatic despite maximally tolerated guideline-directed medical therapy, transcatheter mitral leaflet approximation with MitraClip is safe, provides a durable reduction in MR, reduces the rate of heart failure hospitalizations and improves survival, quality of life and functional capacity during 24-month follow-up,” Stone said. “As such, the MitraClip is the first therapy shown to improve the prognosis of patients with heart failure by reducing secondary MR with left ventricular dysfunction.”
The results differed markedly from the MITRA-FR trial presented last month at the European Society of Cardiology Congress, which showed no significant differences in heart failure or mortality outcomes at one year for patients treated with the MitraClip or medical therapy alone. But that multicenter French trial enrolled patients with less severe MR and more dilated left ventricles, Stone pointed out; left ventricular end-diastolic volume was 135 mL/m2 in MITRA-FR and 101 mL/m2 in COAPT.
Also, Stone said the investigators in COAPT were more stringent about applying maximally tolerated guideline-directed medical therapy to patients. Treatments were more variable in MITRA-FR, which may be more indicative of current real-world practice. Procedural complications were also lower in COAPT (8.5 percent) than in MITRA-FR (14.6 percent), suggesting operator expertise and experience may have also played a role in the improved outcomes.
Applicability on COAPT trial data to everyday practice
The buzz generated by the results of the trial was tempered by the sobering realization that these outcomes are unlikely to be replicated in routine practice without matching the operator experience, medical treatment targets and patient selection achieved in the study setting.
“This was such a well-conducted trial it may be difficult to generalize this to the practicing public,” Leon noted. “The generalizability from the standpoint of operator performance and also the engagement of the heart failure community and ability to be able to work through the heart failure process in the real world is going to be more complex.”
Added Mack: “Regarding the question of generalizability, as well as the expertise of the operators, the second is the adequacy of guideline-directed medical therapy and I think that’s one of the reasons why this trial may be so positive. It’s well-known in the field of heart failure that device therapy is well-affected depending on optimum, guideline-directed medical therapy. So, the message to the community is going to be, if MitraClip is going to be effective, these patients have to be treated with guideline-directed medical therapy.”
The sweet spot for treatment, the investigators indicated, is a patient who maintains moderate to severe MR even after medical treatment but whose ventricles aren’t completely “blown out” or dilated. Stone estimated about 10 percent of the sizable heart failure population is similar to that of the group treated in COAPT.
Insights into pathophysiology of MiutraClip and its use in heart failure
In addition to supporting a potential new treatment for a patient population with few options, Stone said the trial may even help further the understanding of the pathogenesis of heart failure.
“What I think we’ve seen here is that secondary mitral regurgitation is not just a bystander,” he said. “Heart failure experts just thought it was a marker … of a sicker left ventricle, but we’ve seen now that it does contribute to the abnormal pathophysiology of these patients. We didn’t cure patients by fixing their mitral regurgitation—they still had 29 percent two-year mortality—but we did markedly improve their quality of life, readmissions for heart failure and their survival somewhat by at least interrupting that part of the abnormal pathophysiology.”
In the U.S., the MitraClip is currently indicated for the treatment of primary MR for patients who are at prohibitive risk of surgery. Stone believes COAPT could nudge the FDA toward expanding the device’s indication to include secondary MR patients like the ones included in the study.
“I believe that the FDA should act on this data,” he said.