Transcranial sonography predicts functional outcome after stroke thrombectomy
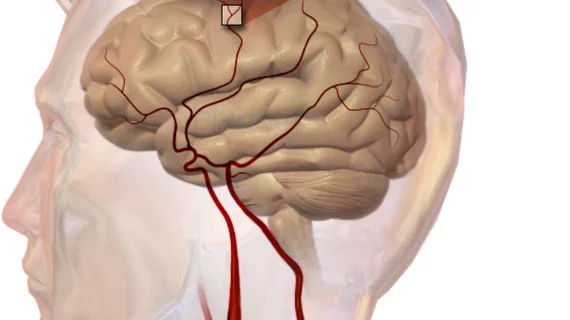
Transcranial duplex sonography (TCD) can assess middle cerebral artery blood flow and provide prognostic information for stroke patients after thrombectomy for large vessel occlusions, suggests a report published Oct. 15 in Stroke.
The study included 215 large vessel occlusion stroke patients, 193 (90 percent) of whom showed successful angiographic recanalization with mechanical thrombectomy (MT). But even among those patients, 36 percent had abnormal cerebral artery hemodynamics upon TCD evaluation—and that group showed a 2.4-fold increased risk of a poor functional outcome at 90 days versus normal TCD flows, after multivariable adjustment. Poor 90-day outcome was defined as a modified Rankin Scale score of 3 or higher.
The researchers—all from the Medical University of Graz in Austria—noted cerebral blood flow changes after thrombectomy have previously been linked to additional complications or shifting prognoses. But most of those studies used arterial spin labeling MRI, which might not be as practical as TCD due to its high technical requirements and prohibited use in unstable patients.
“The present study supports bedside TCD as a modality of interest to monitor cerebral blood flow and to detect abnormal cerebral hemodynamics in the early period after MT,” wrote Markus Kneihsl, MD, and colleagues.
TCD was assessed within 72 hours of thrombectomy for all patients, with a median time of eight hours post-intervention.
Sixty-one percent of patients with abnormal blood flow upon TCD had poor 90-day functional outcomes, compared to 41 percent of those with normal TCD flow. For individuals who didn’t receive successful angiographic recanalization, those with normal TCD flows were more likely to have a favorable 90-day prognosis (30 percent versus 8 percent), although that difference wasn’t statistically significant due to the subgroup’s low numbers.
“The most likely mechanism behind increased (middle cerebral artery) flow velocity is failure of cerebral autoregulation, which appears more likely in patients with large infarcts and may also be associated with hemorrhagic complications because of hyperperfusion,” the authors wrote. “Increased MCA blood flow might have also come from vessel stenosis, but a major contribution seems unlikely as only few patients had also other signs of an underlying MCA stenosis on postinterventional TCD.”
Kneihsl et al. said their analysis was limited by its retrospective design and missing data on some determinants of cerebral blood flow, including collateral status.
“Pathophysiologic assumptions will need to be addressed by larger and prospective studies including serial TCD measurements and parallel information on MCA patency with computed tomography angiography or magnetic resonance angiography and cerebral perfusion,” they wrote.