When should stroke thrombectomy be considered futile?
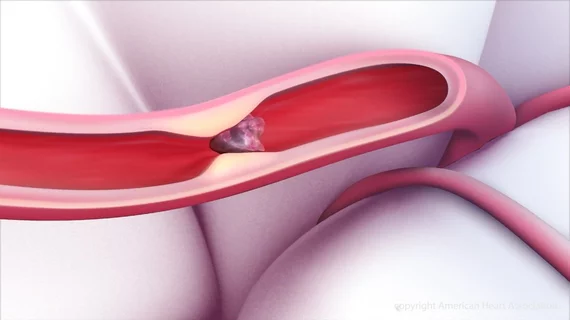
When endovascular thrombectomy procedures for acute ischemic stroke take more than an hour or require more than three attempts to remove the clot, outcomes significantly worsen, according to a study published Feb. 25 in the Journal of the American College of Cardiology.
“Exceeding 60 min of procedure time or 3 aspiration attempts should trigger a careful assessment of the futility and risks of continuing the procedure,” lead author Ali Alawieh, PhD, with the Medical University of South Carolina, and colleagues wrote.
The analysis included 1,359 patients with large-vessel occlusion strokes who were treated with either a stent retriever or direct aspiration thrombectomy at seven U.S.-based comprehensive stroke centers over a five-year period ending March 2018. The average age of the study population was 67 and 51 percent of patients were women. IV tissue plasminogen activator (tPA) was administered in 46 percent of cases.
After multivariate adjustment, a procedure time of less than 30 minutes was linked to a 56 percent increased chance of good functional outcome at 90 days, indicated by a modified Rankin score (mRS) of 0 to 2.
Alawieh et al. noted two specific plateaus regarding procedure time—one after 30 minutes and one after 60 minutes. The rate of good outcomes dropped by 40 percent after a half an hour and dropped about 70 percent after an hour. Rates of post-procedural symptomatic hemorrhage and procedural complications doubled every 26 and 50 minutes, respectively.
The outcomes penalty for repeated thrombectomy passes showed a more linear relationship, the authors found.
“Each thrombectomy pass represents an independent interaction with the vessel with a finite complication rate, so that multiple attempts begin to cumulatively add to the risk profile,” they wrote. “Importantly, the number of attempts demonstrated a linear association with rates of good outcome and increased risk of hemorrhage, which is consistent with recent reports in patients undergoing (aspiration-based or stent retriever) thrombectomy.”
Functional independence (mRS of 0 to 2) was observed in 45 percent of patients with a procedure time below 30 minutes, 33 percent of those with a procedure time between 30 and 60 minutes, and 27 percent of those with a procedure time longer than an hour. Ninety-day mortality rates were also higher among those with intermediate (22 percent) and extended procedure times (39 percent) compared to those who received rapid clot removal in less than 30 minutes (17 percent).
“In patients with procedure time <30 min or 30 to 60 min, fewer attempts but not shorter procedure time were an independent predictor of good outcome, which indicates that in addition to fast recanalization, the use of few recanalization steps was an independent predictor of outcomes in the rapid and intermediate recanalization groups,” Alawieh et al. wrote. “However, in patients with >60 min of procedure time, 1-min increments of procedure time were associated with lower odds of good outcome at 90 days.”
In a related editorial, neurosurgeon Nestor R. Gonzalez, MD, agreed 60 minutes into a procedure might be a good time to “consider the futility of continuing the procedure.” However, he differed with Alawieh and colleagues that the same re-evaluation should take place after three failed thrombectomy attempts.
“At 5 attempts, the cumulative percentage of recanalizations with TICI (Thrombolysis in Cardiac Ischemia) 2b is close to 85%, whereas at 3 attempts, that percentage is 70%,” wrote Gonzalez, with Cedars Sinai Medical Center in Los Angeles. “Also, Figure 1D shows that at 5 attempts, 40% of cases had good outcomes at 90 days.
“Given that recanalization success is the most important predictor of outcome, these data suggest that the rate of complications produced by 2 additional manipulations of the artery would not overcome a potential 15% increase in obtaining recanalization, and that in challenging cases, (more than) 3 attempts of thrombectomy might still be beneficial.”