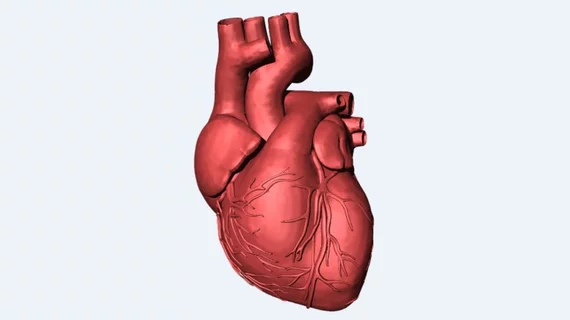
Scientists 3D-print world’s first heart with cells, blood vessels
Researchers at Tel Aviv University in Israel have 3D-printed what they said is the first vascularized heart using a patient’s own cells and biological materials.
Models of hearts and medical devices have been printed in the past to help with procedural planning, particularly in the case of structural or valvular interventions. But this work, published online April 15 in Advanced Science, takes cardiac 3D printing a step further, according to lead author Tal Dvir, PhD, and colleagues.
"This is the first time anyone anywhere has successfully engineered and printed an entire heart replete with cells, blood vessels, ventricles and chambers," Dvir said in a press release. "People have managed to 3D-print the structure of a heart in the past, but not with cells or with blood vessels. Our results demonstrate the potential of our approach for engineering personalized tissue and organ replacement in the future."
Dvir said the organ they produced is the size of a rabbit’s heart but requires the same technology it would take to engineer larger human hearts.
The process involves taking a piece of omental tissue from a patient’s abdomen, reprogramming the cells to become pluripotent stem cells and then converting those into either cardiomyocytes (heart muscle cells) or endothelial cells (for blood vessels). Those cells are then used to form “bioinks,” which are “substances made of sugars and proteins that can be used for 3D printing of complex tissue models,” Dvir said.
Cardiac anatomy was taken from a CT scan of the patient’s heart, which showed the 3D structure of the organ and the orientation of major blood vessels in the left ventricle. Smaller blood vessels—which cannot be imaged with CT—were added to the design using mathematical models and accounting for laws of oxygen diffusion and consumption. With this approach, Dvir et al. wrote that they achieved “an optimal size, distribution, and orientation of the supplemented blood vessels.”
Translating this research into clinical practice one day is a worthy goal for a couple of reasons. For one, people die or get too sick for heart transplants while on the waitlist each year, so another source of production could help alleviate the shortage of organs. Also, transplant recipients require immunosuppressive drugs to prevent organ rejection, but if a heart could be made using bioinks from that same person, those expensive medications could be avoided, Dvir and co-authors wrote.
But much work remains before these benefits can be realized, they acknowledged. Outstanding challenges including finding ways to image and print more complete vasculature, including smaller blood vessels, and efficiently expanding the pluripotent stem cells to enable the creation of larger, functioning hearts.
"We need to develop the printed heart further," Dvir said in the release. "The cells need to form a pumping ability; they can currently contract, but we need them to work together.
“Our hope is that we will succeed and prove our method's efficacy and usefulness. Maybe, in 10 years, there will be organ printers in the finest hospitals around the world, and these procedures will be conducted routinely.”