Mobile stroke units get patients to hospital faster than ambulances
Transport to the hospital via mobile stroke unit—as opposed to standard transit in an ambulance—saved stroke victims 10 minutes and up to 270 million neurons in a study out of the University of Texas Health Science Center at Houston.
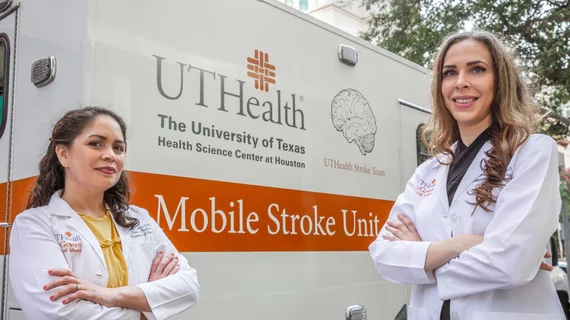
Five years ago, McGovern Medical School at UTHealth was the first center in the U.S. to launch a mobile stroke unit—an ambulance that’s specially equipped to diagnose and treat stroke while patients are en route to their local hospital. On board, an interdisciplinary medical team performs diagnostic imaging and neurological exams to determine whether patients are good candidates for endovascular thrombectomy.
If they determine the patient should undergo thrombectomy, mobile stroke unit teams are able to notify the nearest hospital that they’re on their way, giving on-site physicians a chance to organize and prepare for the procedure before the victim even makes it to the endovascular suite.
“Our mobile stroke unit allows us to bring the hospital to the patient,” Alexandra Czap, MD, a vascular neurology fellow at McGovern Medical School, said in a release. Czap is first author of her team’s recent study, which was published in Stroke.
“We can complete the necessary diagnostic testing and notify the hospital that we are coming so that the appropriate teams can be ready. Going forward, identification of possible thrombectomy candidates on the unit can increase the accuracy of triage and increase the number of patients having the procedure, which we hope will lead to better patient outcomes.”
Part of the ongoing BEST-MSU study, Czap and her colleagues’ research looked at data from 161 patients in Texas who underwent intra-arterial thrombectomy for an acute ischemic stroke between 2014 and 2018. They found patients who were transported to the hospital in a mobile stroke unit received thrombectomy an average of 10 minutes quicker than patients who arrived in an ambulance, potentially saving up to 270 million neurons per patient.
The study also found that, regardless of how they arrived at the hospital, patients saw an overall improvement in endovascular thrombectomy metrics. While it wasn’t their goal to assess those metrics, the authors said it was a significant finding since thrombectomy has just started to be recognized as a standard treatment for stroke within the past five years.
“The quicker we get stroke victims treatment that will restore blood flow, the more brain tissue we can save,” Czap said. “This study shows that mobile stroke units like ours can be effective in streamlining time to treatment, potentially saving neurological function and ultimately improving quality of life in stroke patients.”