AI-based CAD assessments dramatically improve vascular surgery outcomes
Artificial intelligence-based coronary artery disease (CAD) evaluations can improve the long-term survival of patients undergoing major vascular surgery to treat their peripheral artery disease (PAD), according to new data published in the Journal of Vascular Surgery.[1]
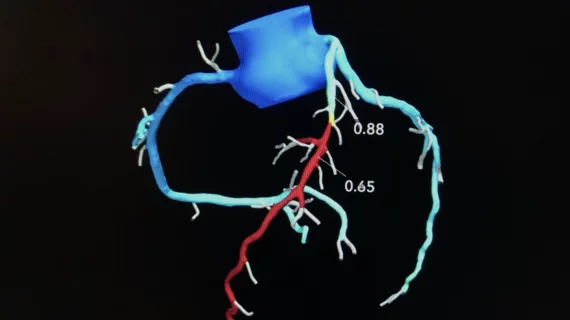
The study’s authors noted that many PAD patients also present with CAD, increasing their risk of adverse surgical outcomes, but the CAD is often asymptomatic. They aimed to learn if evaluating PAD patients with HeartFlow’s noninvasive FFRCT Analysis technology, which uses AI to evaluate coronary CT angiography (CCTA) results for warning signs of CAD, could help care teams provide better vascular care and lead to improved clinical outcomes.
Researchers explored data from more than 500 PAD patients who presented with no history of CAD or CAD symptoms and underwent elective carotid, peripheral or aneurysm surgery. All patients were treated at a single center from 2017 to 2019.
While 288 patients were assessed using HeartFlow’s FFRCT Analysis technology and then treated with postoperative coronary revascularization as needed, the remaining 234 patients underwent standard care without the use of FFRCT Analysis or postoperative coronary revascularization. The two groups were comparable in age, gender and comorbidities.
Overall, signs of asymptomatic lesion-specific coronary ischemia were identified in 65% of patients assessed with FFRCT Analysis. These patients were then treated with selective revascularization after undergoing vascular surgery.
After five years, patients in the FFRCT group were associated with a 63% lower risk of all-cause death, including an 89% reduction in cardiovascular death. FFRCT evaluations were also linked to a significantly lower risk a major adverse cardiovascular event, a composite outcome that includes death, myocardial infarction and stroke.
“These data show that there is a role for coronary revascularization in the management of CAD in vascular surgery patients and that sole reliance on medical treatment and risk factor control has been insufficient,” wrote first author Dainis K. Krievins, MD, PhD, a vascular surgery specialist at Pauls Stradins Clinical University Hospital in Latvia, and colleagues. “Although the diagnosis of silent coronary ischemia in our study was made preoperatively, the long-term benefit of fewer adverse coronary events and improved survival was achieved with postoperative coronary revascularization. It is possible that a strategy of postoperative diagnosis of coronary ischemia coupled with ischemia-targeted coronary revascularization may be equally effective.”
HeartFlow issued a statement about this analysis, highlighting the positive impact its technology had on patient care for these PAD patients presenting for surgery.
“Despite advances in peripheral vascular disease treatment, the mortality rate following vascular surgery remains distressingly high,” Christopher Zarins, MD, HeartFlow’s senior vice president of medical affairs and one of the study’s co-authors, said in the statement. “With our AI-powered approach, HeartFlow addresses a critical and longstanding clinical challenge by noninvasively determining the presence of significant CAD and facilitating its effective treatment. Ultimately, the result is that patients with atherosclerotic disease can receive access to a more accurate diagnosis and treatment, dramatically reducing their likelihood of death.”