CRT-D associated with major improvements among older HFrEF patients
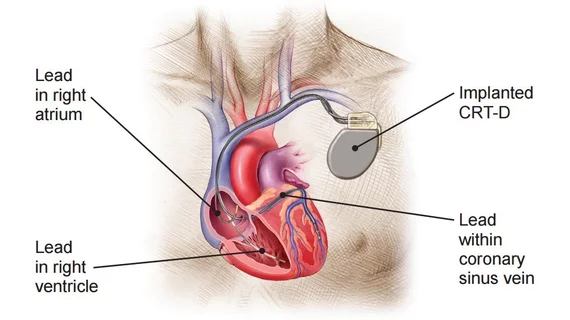
Cardiac resynchronization therapy with a defibrillator (CRT-D) is associated with “significant improvements” in mortality and heart failure (HF) hospitalization rates among older Medicare patients, according to new research published in JACC: Heart Failure.[1]
“Despite the transition of the population of patients with HF to one that is older and more comorbid, evidence that supports that most HF therapies were derived in younger, healthier patients,” wrote first author Emily P. Zeitler, MD, MHS, a cardiovascular medicine specialist with Dartmouth-Hitchcock Medical Center in New Hampshire, and colleagues. “Evidence that supports the implantable cardioverter-defibrillator (ICD) and CRT for eligible subjects largely comes from high-quality randomized controlled trials, but the average age of randomized subjects was 64-66 years, and the enrollment of older patients was limited. This evidence is reflected in age-agnostic guidelines by relevant professional societies. Indeed, the benefit of CRT in older patients has been identified as a major gap in knowledge and as a priority for future research.”
Zeitler et al. examined data from nearly 14,000 fee-for-service Medicare beneficiaries with a confirmed diagnosis of HF with reduced ejection fraction (HFrEF). All patients were over the age of 65 and underwent CRT-D or ICD implantation from January 2008 to August 2015. Overall, the authors found, the CRT-D group more likely to be white, female and present with left bundle branch block.
One-year mortality was on the high end for all patients. However, among patients 75 years old and older, CRT-D implantation was associated with a lower risk of mortality than ICD implantation.
Also, among patients 85 years old and older, CRT-D implantation was associated with a lower risk of HF hospitalization. This difference was significant when evaluated using a Kaplan-Meier survival analysis.
Zeitler’s team also found that device-related complications were “relatively frequent” among all patients, but ICD patients 85 years and older faced the highest risk of complications. The lowest risk of complications, meanwhile, was seen in CRT-D patients 65 to 74 years old.
“Bleeding was the most common complication, occurring in 5% to 8% of patients, depending on age and device complexity,” the authors wrote. “Most individual complications, however, occurred too infrequently to report because of Centers for Medicare and Medicaid Services (CMS) suppression rules, which limit the ability to report outcomes in small groups to reduce the risk of inadvertent patient identification.”
Today’s HFrEF population is getting older and older, the researchers noted, causing more of them to present with other health issues that often elevate the risk of complications following CRT-D or ICD implantation. With this in mind, they said, “the inclusion of older patients in future randomized clinical trials of HF interventions would improve understanding of therapies in this growing population.”
Related Heart Failure Content:
How COVID-19 vaccination affects the risk of ED visits for cardiac, respiratory issues
Abbott implantable heart failure monitor gains expanded FDA approval
AEE use during CIED procedures for HFrEF patients not always cost-effective
Find more heart failure content
Find more electrophysiology content
Reference