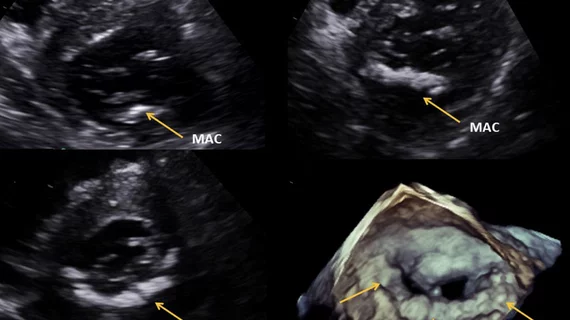
Mitral annulus calcification more than doubles a patient’s risk of heart valve disease
Patients with mitral annulus calcification (MAC) are more than twice as likely to present with mitral valve dysfunction (MVD), according to a new analysis published in Mayo Clinic Proceedings.[1] MAC is also linked to a higher risk of cardiovascular disease (CVD) and all-cause mortality.
The study’s authors retrospectively reviewed data from more than 24,000 patients who were treated in 2015 at Mayo Clinic in Rochester, Minnesota. All patients underwent transthoracic echocardiography (TTE) at the time of treatment. The median follow-up time was three years.
Based on the TTE findings, researchers determined that 23% of patients presented with MAC. MAC patients had a much older mean age (75 years old) than patients without MAC (60 years old).
MVD, defined as mitral stenosis “of moderate or greater severity,” was identified in 16% of MAC patients and 6.6% of patients without MAC.
“MAC has been known to be associated with CVD and mortality, but we did not previously appreciate the strength of this relationship even after adjustment for multiple clinical and echocardiographic variables,” corresponding author Patricia Pellikka, MD, a Mayo Clinic cardiologist, said in a statement.
The authors also noted that mitral stenosis, aortic stenosis, prior aortic valve replacement, left ventricular outflow tract obstruction and renal dysfunction were all associated with a greater risk of MAC. Mitral regurgitation, meanwhile, was not associated with MAC in any way.
“Patients with calcification more commonly had not only MVD, but also aortic valve disease,” Pellikka said. “For clinicians, suspicion for valve diseases should be increased and evaluations carefully performed for patients with MAC.”
A grant from Abbott Structural Heart did fund this analysis, and one co-author has a previous relationship with Abbott. No other authors reported any relationships relevant to their study.
Related Structural Heart Disease Content:
Transcatheter PVL closure linked to lower 30-day mortality than surgery
Left bundle branch block after TAVR hurts outcomes, even when no permanent pacemaker is required
New data on cardiac damage before and after AVR suggests earlier treatment may be beneficial
Reference: