Key interventional cardiology takeaways from the SCAI 2022 conference
Here are some key interventional cardiology takeaways from sessions presented at the Society for Cardiovascular Angiography and Interventions (SCAI) 2022 annual meeting in May. The society recently highlighted these points in a newsletter to its members.
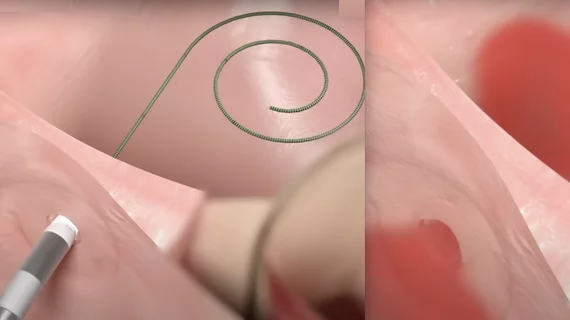
No-implant interatrial shunt for heart failure shows promising efficacy
Early clinical evaluation of the Alleviant System to treat heart failure patients with preserved and reduced ejection fraction (HFpEF and HFrEF) demonstrated procedural safety and feasibility with a promising efficacy signal through six months.
The procedure creates an atrial septal defect (ASD) to help offload left atrial pressure in heart failure patients with both reduced and preserved ejection fraction. The Allegiant device creates a 7 mm ASD with electrocautery and leaves no hardware behind. The ASD was durable and present several months after the index procedure. Patients had lower pulmonary pressures with exercise testing and an improvement in quality of life, said Brian C. Kolski, MD, interventional cardiologist, Orange County Heart Institute, who reviewed the study results. He said in order to recommend this study in heart failure patients, there will likely need to be a randomized sham procedure study.
Updated safety assessment of femoropopliteal treatments with paclitaxel-coated devices
New long-term data from the SAFE-PAD study found no meaningful difference in survival between patients treated with a paclitaxel drug-coated device (DCD) and those treated with a non-drug coated device (NDCD) for up to six years after the index procedure. This was regardless of the patient’s mortality risk and device type.
The SAFE-PAD study was created in collaboration with the U.S. Food and Drug Administration (FDA) to evaluate the long-term safety of paclitaxel-coated devices compared with non-paclitaxel-coated devices for femoropopliteal artery revascularization among a broad, real-world population of patients with PAD. This was done because of a meta analysis study published in late 2017 that appeared to show a higher mortality signal in patients treated with paclitaxel-coated devices. The study was designed to show if there was any increase in adverse events for deaths, explained Chadi Alraies, MD, MPH, medical director, cardiac catheterization laboratory, director, interventional cardiology research, Detroit Medical Center, who summarized the study.
There remained no evidence of harm associated with DCDs, Alraies said. He explained the findings were robust in sensitivity analyses and consistent across all subgroups, in particular those at the lowest risk of mortality.
Sex differences in clinical characteristics, management and outcomes of STEMI patients with COVID-19
The latest analysis from The North American COVID-19 Myocardial Infarction (NACMI) Registry at SCAI showed clinical characteristics and management strategies differ by gender, but in-hospital mortality rates remained high among both groups.
Of the 585 patients enrolled from March 1, 2020, to December 31, 2021, 26% were female and 74% were men. Women were significantly older, had higher rates of diabetes, stroke and statin use on admission. Women were less likely to present with chest pain versus men, at 47% versus 59%, respectively. Women presenting with STEMI were less likely to have identifiable culprit lesion, at 67% versus 82%, on coronary angiography, explained Gary S. Ledley, MD, FSCAI, Tower Health, who summarized the study findings.
The primary trends and results of NACMI were presented at the American College of Cardiology (ACC) annual meeting in April. Watch the VIDEO: Vaccines boosted survival among STEMI patients with COVID-19, an interview with Santiago Garcia, MD, lead author of the study and director of the structural heart program at The Christ Hospital in Cincinnati, Ohio.
Clopidogrel monotherapy vs. aspirin monotherapy for chronic maintenance beyond 12 Months after PCI
This real-world study looked at the safety and effectiveness of clopidogrel versus aspirin monotherapy beyond 12 months after percutaneous coronary intervention (PCI) in high-risk bleeding patients during the chronic maintenance period. Clopidogrel monotherapy was associated with a reduced risk of net adverse clinical events (NACE; all-cause death, MI, stent thrombosis, stroke, or BARC type 2, 3, or 5 bleeding) and MACCE (death, MI, stent thrombosis, stroke), and a numerical decrease in major or clinically relevant nonmajor bleeding (BARC type 2, 3, or 5 bleeding), compared with aspirin monotherapy.
DAPT (dual antiplatelet therapy) is a cornerstone in the treatment of patients after PCI and ACS. After the course of DAPT is completed, patients are typically managed long term with aspirin as a single antiplatelet, explained Michael P. Savage, MD, MSCAI, director, cardiac cath lab, Jefferson University, in his summary.
This study from the Chinese Fuwai Registry included 7,392 patients who were at high risk of bleeding and thrombosis. They were event free on DAPT one year post PCI. Of these, 3,690 were continued on aspirin monotherapy and 1,540 were continued on clopidogrel monotherapy. The outcomes of these two groups were assessed between 12- and 30-months post PCI. Cardiovascular events were lower in the clopidogrel group, but there was no significant difference in bleeding between the two drugs.
Distal vs. proximal radial artery access 30-day outcomes of the DIPRA study
Initial findings from the Distal versus Proximal Radial Artery Access for Cardiac Catheterization and Intervention (DIPRA) study evaluated outcomes of hand function and effectiveness of conventional proximal radial artery (PRA) access compared to distal radial artery (DRA) access for cardiac catheterization. At 30 days, distal radial artery access is safe and is not associated with significant hand dysfunction, said Jordan Safirstein, MD, FSCAI, director of transradial intervention at Morristown, Atlantic Health, who reviewed the study.
The distal radial artery access approach allows the operator to pronate the left hand and work from the right side of the table yielding a clear ergonomic advantage for both patient and operator, Safirstein explained.
The distal radial approach is a relatively new access technique which gained popularity initially through social media, but has never been directly compared to standard radial approach in terms of safety or procedural success rate, in a randomized fashion. DIPRA is a single center, prospective randomized control trial that enrolled 300 adults at Baylor Scott and White Health - the Heart Hospital Plano.
The safety and drawbacks of DRA are not well described, so this study used grip strength, pinch strength and a QuickDASH survey score to assess changes in hand function and will be repeated at 12 months.
The primary outcome was a composite of hand function change. The DRA group demonstrated worsening hand function, but not to a statistically significant degree. Secondary endpoint of pinch grip strength was significantly worse in the DRA group at 30 days (DRA -0.2 kg [95% CI -1.2, 0.5] vs. PRA 0 kg [95% CI -0.9, 0.9]; p=0.05). There was no significant difference in the secondary endpoint of grip strength at 30 days.
Rates of bleeding were similar in both groups (DRA 0% vs. PRA 1.4%, p=0.25). Rates of procedural success were similar in both groups as well (DRA 96.7% vs. PRA 98%; p=0.72).
One-year outcomes in an expanded cohort of patient with the Harmony transcatheter pulmonary valve
This was a study of one-year outcomes in the largest cohort to date of Harmony transcatheter pulmonary valve (TPV) patients with congenital heart disease (CHD) and severe pulmonary regurgitation (PR). The data show Harmony TPV patients had favorable clinical and hemodynamic outcomes, confirming earlier results and demonstrating continued device safety and effectiveness across studies and valve types at one year.
Disorders involving the right ventricular outflow tract (RVOT) and main pulmonary artery (MPA) are the most common issues encountered in congenital heart disease, particularly in Tetralogy of Fallot, wrote Dennis W. Kim, MD, PhD, FSCAI, a pediatric cardiologist at Children's Healthcare of Atlanta, in a summary of the study.
The study included 106 Harmony TPV implants evaluated, representing three variations of the Harmony TPV system, The 6 month data revealed no mortality and 87.5% freedom from transcatheter pulmonary valve dysfunction. Over 90% of implanted valves had none/trace paravalvular leak.
Kim said transcatheter pulmonary valve replacement systems potentially allow for avoidance of repeat open surgical procedures in a population of patients where repeated sternotomies were previously the only option.
Trends of chronic total occlusion PCI from the PROGRESS-CTO International Registry
A new analysis of PROGRESS-CTO (PROspective Global REgiStry for the Study of Chronic Total Occlusion Intervention) shows an increase in the success and efficiency of CTO PCI without an increase in major adverse cardiac events (MACE).
Since the inception of the CTO PCI registry, there have been 10 years of data collected on 10,019 patients treated at 40 centers. The techniques and, thus, outcomes for CTO PCI have evolved over time. The large volume, prospective data presented in this publication provides insight into real-world in-hospital trends and outcomes, explained Allison G. Dupont, MD, FSCAI, interventional cardiologist, Northside Hospital Cardiovascular Institute, Atlanta, in her review of the study.
She said it is no surprise with the advancement of techniques in CTO PCI that the technical success rate for these interventions has increased over time. In 2016, the rate of technical success was 81.6%, but by 2021, this had increased to 88.1%.
The RCA was most commonly treated (53%) with the LAD and left circumflex less commonly targeted at 26% and 19%. Contrast volume, radiation dose, fluoroscopy time and procedure time have continued to decrease over time as operators become more proficient in these cases, according to study data.
The majority of successful CTO lesion crossing was done with antegrade wire escalation strategy (55%). Only 19% were crossed retrograde and 12% antegrade dissection re-entry. Successful crossing with antegrade wire escalation strategy has increased from 46% in 2016 to 61% in 2021.
Importantly, the rate of in-hospital major adverse cardiac events (MACE) remains low (2.1%) without significant changes over time, despite increasing lesion complexity.
Intravascular lithotripsy for peripheral artery calcification one-year outcomes
One-year outcomes from the Disrupt PAD III Trial comparing intravascular lithotripsy (IVL) with a drug-coated balloon (DCB) to percutaneous transluminal angioplasty (PTA) with a DCB revealed consistent safety and effectiveness of IVL with durable patency.
The one-year data demonstrated the consistent safety and durability of IVL in treating Heavily calcified femoropopliteal lesions. The powered secondary endpoint of primary patency at 1-year was significantly higher in the IVL arm (80.5% vs. 68.0%, p=0.017) and remained favorable through two years (Kaplan-Meier estimate: 74.4% vs. 57.7%, p=0.005). Freedom from clinically driven-TLR (IVL: 95.7% vs PTA: 98.3%, p=0.94) and restenosis (IVL: 90.0% vs PTA: 88.8%, p=0.48) were similar between the two groups at 1-year. Moreover, bail-out stenting was significantly lower in the IVL group (4.6% vs 18.3%, p<0.0001) which can help preserve future treatment options in claudicants with severe femoropopliteal calcification.
It remains to be seen how IVL compares to other modalities such as atherectomy and whether the primary patency remains superior in longer term follow-up, explained study reviewer Luai K. Tabaza, MD, FSCAI, interventional cardiologist, Virtua Health, Marlton, New Jersey.