FDA approves trial for new type of thermal-ablation system to treat ventricular arrhythmias
The U.S. Food and Drug Administration (FDA) has approved a clinical trial to evaluate the safety and efficacy of a new type of ablation catheter for patients with ventricular tachycardia (VT) resistant to conventional anti-arrhythmic drugs or standard electrophysiology (EP) ablation procedures.
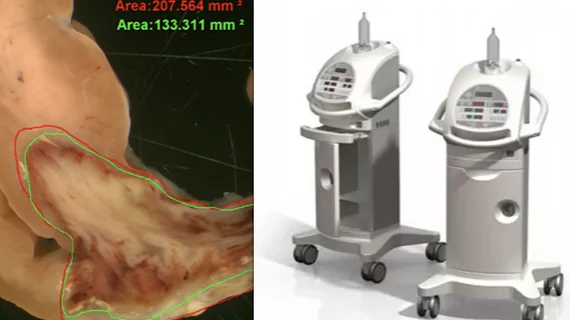
The open-label, single-arm interventional trials will evaluate the Thermedical SERF thermal ablation system with the Durablate Catheter. SERF ablation provides a new form of biological heat transfer designed to be more efficient than conventional ablation methods, the vendor said. It delivers energy with a high level of accuracy to better control the ablation size and treat tissue deeper in the heart wall where life-threatening arrhythmias that cause VT are often located.
“We are grateful to the FDA for the rapid approval of this pivotal trial to evaluate our Saline Enhanced Radiofrequency (SERF) Ablation System in patients who have run out of treatment options for their VT episodes and who suffer from extremely poor quality of life,” explained Michael Curley, PhD, FHRS, in a statement. He is co-founder and CEO of Thermedical, and senior author of the first-in-man multi-center trial evaluating SERF with the Durablate catheter, published in Circulation: Arrhythmia and Electrophysiology.[1] “In our recent multi-center trial, 31 of 32 participants experienced immediate elimination of their clinical VT at the end of the procedure, and therapies such as shock or pace regulation were reduced by 89% during the five-month follow-up in these patients.”
The Mayo Clinic in Rochester, Minn., will be the first of up to 25 investigational sites in North America to enroll patients in the larger clinical trial. Douglas Packer, MD, a cardiac electrophysiologist at Mayo Clinic, is the principal investigator. To date, additional sites are planned for Birmingham, Boston, Charleston, Montreal, Nashville, Philadelphia and Quebec City. The trial will enroll 154 participants with recurrent, sustained, monomorphic VT that is resistant to drug therapy and conventional catheter ablation. The trial participants will have a SERF ablation procedure, with follow-up at seven days, one month, three months, and six months.
The FDA designed the Thermedical SERF Ablation System as a Breakthrough Technology in part because there is currently no approved device that specifically treats this patient population.
Implantable Cardioverter Defibrillators (ICDs) are the current treatment for patients suffering from VT. During a VT episode, the ICD delivers energy to the heart muscle via a powerful shock or antitachycardia pacing to help the heart beat normally again. Today, VT patients with ICDs who experience VT episodes may be treated with conventional RF ablation, a lengthy procedure with a moderate success rate of approximately 50%.