New recommendations for cardiac CT in cardio-oncology imaging
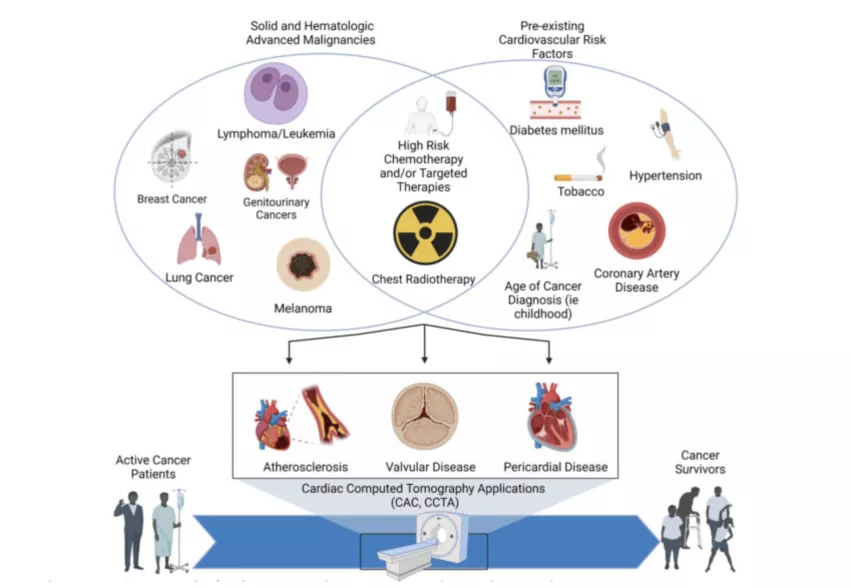
The Society of Cardiovascular Computed Tomography (SCCT) published an expert consensus statement that provides guidance on the use of cardiac CT (CCT) in the care of cardio-oncology patients. Cardio-oncology is a rapidly growing sub-specialty of medicine, but there is very limited guidance on the use of CCT.
Published in Journal of Cardiovascular Computed Tomography (JCCT) and endorsed by the International Cardio-Oncology Society (ICOS),[1] the statement was written with the intent of filling gaps in recommendations from prior consensus statements and guidelines in regards to the use of CCT in cardio-oncology.
This expert consensus statement comprised of a multidisciplinary collaboration of experts in cardiology, radiology, cardiovascular imaging, cardio-oncology and radiation oncology from SCCT aims to summarize current evidence for CCT applications in cardio-oncology and provide practice recommendations for clinicians.
“The importance of this document is that it provides expert consensus recommendations in cancer patients and survivors, an area with paucity of data and lack of guidance by guidelines and standards in the field of cardio-oncology,” explained Juan Lopez-Mattei, MD, FSCCT, lead author and medical director of cardiac imaging at Lee Health Heart and Vascular Institute in Fort Myers, Florida, in a statement.
Cancer patients and survivors have significantly increased cardiovascular risk when compared with non-cancer patients, he said. “The intentions of many of our recommendations are to be able to identify subclinical atherosclerotic cardiovascular disease (ASCVD) in these patients and to initiate promptly and appropriately preventive treatments.”
The writing group placed emphasis on reviewing prior recent non-gated chest CT scans if available to assess for subclinical presence of ASCVD and further cardiovascular risk assessment (qualitative or quantitative) using the CAC-Data Reporting System (CAC-DRS).
According to Lopez-Mattei, the key takeaway for the clinical cardiologist, oncologist and radiation oncologist is to use pre-existing non-gated chest CT scans from cancer patients and survivors to assess for the presence of coronary artery calcium (CAC), and either promptly treat or refer to a cardio-oncologist.
Another key use of CCT angiography (CCTA) in cardio-oncology is to rule out obstructive coronary artery disease (CAD) in patients with troponin elevation, when an alternative diagnosis for myocardial injury other than coronary thrombosis is more likely. This is particularly true with some types of chemotherapy agents are being used. CCTA can also rule out obstructive CAD as the etiology of decreased left ventricular systolic function/cardiomyopathy to better understand if the caner treatment is the cause of myocardial impairment.
For radiologists and nuclear medicine physicians, the guidance advises to start mentioning presence or absence of CAC in reports, and to start considering assessment of CAC burden quantitatively or qualitatively in non-contrast non-gated scans.