Infection, heart failure the most common reasons for early mortality after transvenous lead removal
The most common causes of mortality during transvenous lead removal (TLR) in patients with cardiac implantable electronic devices (CIEDs) are infection and decompensated heart failure, according to new research published in JACC: Clinical Electrophysiology.[1]
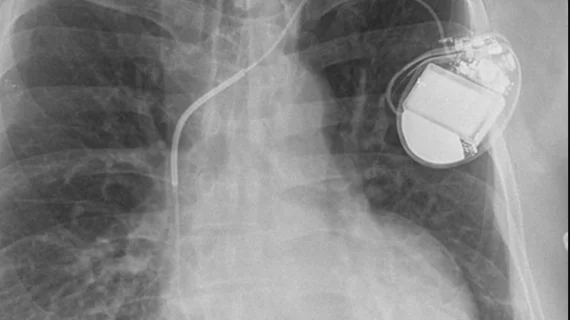
“The CIED has been widely used in the past decades, with an estimated 1.25 million permanent pacemakers being implanted worldwide yearly, and the use of CIEDs continues to increase,” wrote first author Justin Z. Lee, MD, an electrophysiologist with Cleveland Clinic who was with Mayo Clinic in Arizona at the time of the study. “This has also led to an increase in device-related complications and a growing need for lead removal. Although the extraction technique has improved, it remains a technically challenging procedure with the potential for life-threatening complications.”
Lee et al. examined data from more than 2,300 adult patients with CIEDs who underwent TLR from Jan. 1, 2001, to Jan. 1, 2021. The mean patient age was 64 years old, and 65% of patients were men.
Overall, all-cause mortality after 30 days was 3% over the study’s 20-year study period. Infection (42%) was the No. 1 cause of 30-day mortality, followed by decompensated heart failure (17%), procedure-related mortality (10%), sudden cardiac arrest (7%) and respiratory failure (6%). Mortality specifically related to the TLR procedure was seen in just 0.3% of patients.
In addition, the authors found, 33% of deaths included in this study happened when the patient had already been discharged. While 43% of those patients were readmitted before they died, another 35% died from home or a nursing facility and 22% died in hospice.
“Most mortality was not related to the TLR procedure,” the authors wrote. “Therefore, to reduce the 30-day mortality in TLR, increasing research in pre-operative and post-operative management is important.”
The average time from CIED procedure to TLR was 11 days. Identifying the need for TLR more quickly may be one way to lower the mortality rate among patients who need TLR, the researchers wrote, but they also said it would be “impossible to draw any conclusions from the present study regarding optimal timing.”
Previous research had determined that heart failure and chronic kidney disease were both linked to a higher risk of mortality after TLE. This latest analysis, however, found that older age and chronic obstructive pulmonary disease are two additional “significant predictors” that researchers should keep a close eye on going forward.
“Further prospective studies are necessary to evaluate therapeutic strategies to improve post-procedural infection and heart failure outcomes in patients undergoing TLR,” the authors concluded.