Increased AFib screening improves bradyarrhythmia detection—but is it a mixed blessing?
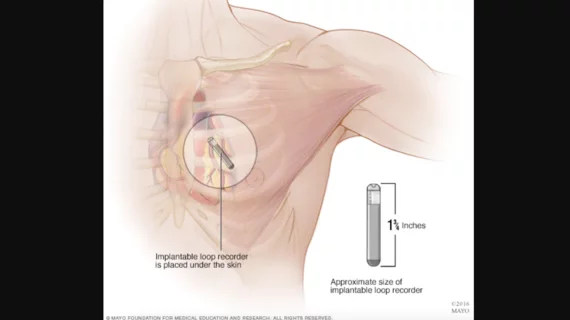
The increased use of implantable loop recorders (ILRs) is associated with identifying more bradyarrhythmias such as bradycardia, according to new findings published in JAMA Cardiology.[1] However, researchers noted, this largely led to the detection of more asymptomatic bradyarrhythmias; clinical outcomes did not significantly improve.
“Recent years have seen an increased interest in heart rhythm monitoring and a surge of new technologies to detect arrhythmias,” wrote first author Søren Zöga Diederichsen, MD, PhD, a cardiologist with Copenhagen University Hospital-Rigshospitalet in Denmark, and colleagues. “Much interest has focused on tools to detect subclinical atrial fibrillation (AFib) or help manage or diagnose patients with palpitations, whereas data on sinus node dysfunction (SND) and atrioventricular block (AVB) are scarce.”
Diederichsen et al. examined data from a randomized clinical trial of nearly 1,500 older patients with no prior history of AFib who underwent ILR screening. All patients were at least 70 years old and had a confirmed diagnosis of hypertension, diabetes, heart failure or prior stroke. More than 4,500 control patients, who underwent normal care instead of ILR screening, were also included in the study.
Overall, after a median follow-up period of 64.5 months, bradyarrhythmias were identified in 3.8% of control patients and 20.8% of ILR patients. SND and low-grade AVB were identified in 1.5% and 0.8% of control patients, respectively, and 13.6% and 4.1% of ILR patients, respectively.
“Definitely symptomatic” bradyarrhythmias were seen in 2.2% of control patients and 2.7% of ILR patients. Bradyarrhythmias “with possible symptoms” were seen in 0.7% of control patients and 1.5% of ILR patients. “Completely asymptomatic” bradyarrhythmias, on the other hand, were seen in 0.9% of control patients and 16.6% of ILR patients.
Additional findings from the team’s analysis:
- Pacemakers were implanted in 2.9% of control patients and 4.5% of ILR patients.
- Syncope occurred in 2.7% of control patients and 2.2% of ILR patients.
- Sudden cardiovascular death occurred in 1.1% of control patients and 1.2% of ILR patients.
- Bradyarrhythmias were seen in 19.1% of patients with AFib, but just 5.8% of patients without AFib.
- Bradyarrhythmias were linked to subsequent syncope, cardiovascular death and all-cause death.
“Long-term continuous monitoring led to a six-fold increase in bradyarrhythmia diagnoses and a significant increase in pacemaker implantations compared with usual care, but no change in the risk of syncope or sudden death,” the authors wrote. “The findings indicate that incidentally detected bradyarrhythmia may be a risk marker but is often not a disease itself.”
Read the full analysis here.
Can increased AFib screening be a mixed blessing?
In a separate commentary piece, also published in JAMA Cardiology, two electrophysiology specialists offered their own perspective on these findings.[2]
Co-authors Mark H. Schoenfeld, MD, of Yale University School of Medicine and Kristen K. Patton, MD, of the University of Washington School of Medicine, noted that ILR screening was associated with a “significantly higher pacemaker implantation rate” without improving key clinical outcomes.
“The risk of overdetection and overtreatment with pacemaker therapy in patients with ILR-detected bradycardia cannot be ignored,” the two authors wrote. “Fundamentally, what constitutes a sufficient bradycardia warranting intervention in the asymptomatic patient is unclear.”
This study also helped show that cardiologists may need to “reconsider the medical context in which bradycardia occurs,” Schoenfeld and Patton explained. When bradyarrhythmias are identified, it will be important to remember going forward that they may represent a sign of a much more serious heart condition.
Overall, the two authors concluded that the increased use of monitors such as ILRs represents something of a “mixed blessing” for heart teams going forward.
“Clearly, sensitivity for life-threatening arrhythmic conditions is enhanced with more monitoring, which has obvious benefit for our most fragile populations,” they wrote. “Conversely, this advantage is a double-edged sword, as it comes intertwined with the manifest financial and personal costs of overtreatment. Moreover, the genuine impact of these data may transcend even this essential management issue as they illustrate the changing nature of diagnosis and prognosis due to advances in technology.”