Next-generation TAVR valve delivers strong outcomes, reduced PVL after one year
The SAPIEN 3 Ultra (S3U) transcatheter heart valve from Edwards Lifesciences is associated with strong one-year transcatheter aortic valve replacement (TAVR) outcomes, according to new findings published in EuroIntervention.[1] This includes significant reductions in paravalvular leak (PVL) when compared to the previous transcatheter heart valve from Edwards, the SAPIEN 3 (S3).
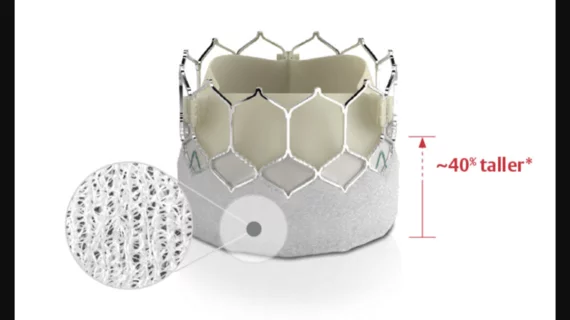
“Over the past several years, the technological advancement of new-generation TAVR devices has been focused on the minimization of PVL,” wrote first author Stefano Cannata, MD, with the Mediterranean Institute for Transplantation and Advanced Specialized Therapies in Palermo, Italy, and colleagues. “In fact, the latest-generation balloon-expandable transcatheter heart valve, the S3U, incorporates an outer skirt made from a textured polyethylene terephthalate, which is 40% higher than that of the S3, to achieve better sealing. Initial data about the early post-implantation performance of the S3U are promising, especially in terms of a reduced PVL rate. However, there are limited data about the longer-term clinical outcomes and hemodynamic performance of the S3U.”
The group’s analysis focused on data from the SAPIEN 3 Ultra registry, which included TAVR patients treated at one of 12 European facilities from October 2016 to December 2020. While more than 500 TAVR patients were treated with the S3U valve, more than 1,100 TAVR patients were treated with the S3 valve.
Edwards Lifesciences did not fund or contribute to this analysis in any way.
Overall, the device success rate was 90.6% for the S3U group and 92.2% for the S3 groups. Diving deeper into the data, all-cause mortality after one year was 4.9% for the S3U group and 6.3% for the S3 group. Also, the composite outcome of all-cause mortality, disabling stroke and heart failure hospitalization after one year was 6.6% for the S3U group and 9.5% for the S3 group.
Mild PVL, meanwhile, was seen in 17.4% of patients in the S3U group and 27.1% of the S3 group. Moderate or greater PVL was seen in 0.8% of patients in the S3U group and 3.1% of the S3 group. This trend was maintained after one year.
“Our study results show a very low rate of PVL associated with the S3U suggesting that the main distinguishing features of the new-generation S3U have a significant preventive role,” the authors wrote. “The absence of PVL was significantly higher in the S3U compared to the S3 group at discharge and, more importantly, the results were confirmed at one-year follow-up.”
Cannata et al. noted that additional research is still needed to help determine if reduced PVL rates have a long-term impact on patient outcomes.
Read the full study here.