Redo TAVR appears feasible for most patients with supra-annular, self-expanding Evolut valves
When transcatheter aortic valve replacement (TAVR) with a supra-annular, self-expanding valve fails, is redo TAVR a feasible treatment option or will the patient require surgery? A team of cardiologists and surgeons aimed to find out, sharing its findings in EuroIntervention, the official journal of EuroPCR and the European Association of Percutaneous Coronary Interventions.[1]
The study’s authors examined data from 204 patients who underwent TAVR with an Evolut R or Evolut PRO valve from Medtronic, simulating redo TAVR with either a balloon-expandable SAPIEN 3 (S3) valve from Edwards or another Evolut valve. All data originally came from the Evolut Low Risk Trial, which was sponsored by Medtronic.
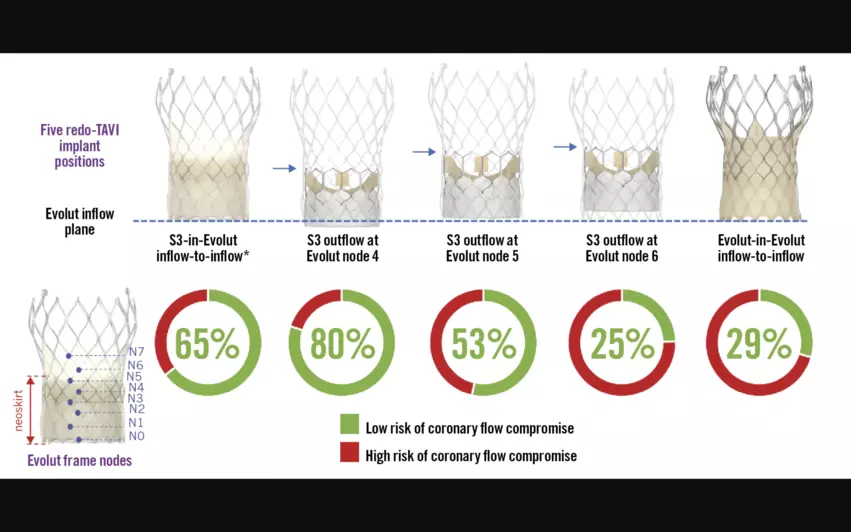
Redo TAVR involves implanting a new transcatheter aortic valve (TAV) into the failed TAV. Five different techniques for redo TAVR were included in this study: S3-in-Evolut inflow-to-inflow, S3 outflow at Evolut node 4, S3 outflow at Evolut node 5, S3 outflow at Evolut node 6 and Evolut-in-Evolut inflow-to-inflow. CT imaging results were consulted before and after each redo TAVR procedure.
Overall, the risk of coronary flow compromise was lowest—20%—when the S3 outflow was positioned at node 4 of the Evolut valve. On the other hand, that risk was highest—75%—when the S3 outflow was positioned at node 6 of the Evolut valve. This confirmed that, yes, redo TAVR with these supra-annular, self-expanding valves is feasible—as long as operators use the right technique.
“Structural heart teams have to discuss lifetime management at the time of the initial TAVR now that younger patients, with longer life expectancies, are being offered TAVR,” lead author Kendra Grubb, MD, an associate professor in the department of surgery at Emory University in Atlanta, told Cardiovascular Business. “We have promised our patients that we can ‘just put another one inside’ without data to support this claim. This study shows that, 80% of the time, we should be able to safely put another valve inside a failed Evolut.”
Even when the S3 outflow was placed at node 4 of the Evolut, the authors noted, women and patients with a higher BMI were both linked to a higher risk of coronary flow compromise.
“This was not surprising as one would assume women, having a smaller aortic root anatomy, would be at higher risk,” Grubb her co-authors wrote. “Indeed, when evaluating native CT anatomical measurements, smaller aortic annulus dimensions were significant predictors associated with a higher risk of coronary flow compromise.”
The authors also noted that a shallower implantation depth was directly tied to a higher coronary flow compromise risk. The “optimal” cut-off point for implantation depth of the index Evolut was found to be 2.3 mm at the non-coronary cusp, but due to the small sample size, this cut-off point may not necessarily be ideal for all patients.
“A preprocedural CT planning approach of the index TAVR is necessary for every patient to facilitate future coronary access after redo TAVR,” the authors explained. “Understanding the native anatomy and implanting an appropriately sized index Evolut valve at an optimized implantation depth will facilitate future coronary access after redo TAVR.”
Both the original Evolut Low Risk Trial and this new analysis were sponsored by Medtronic. Grubb and other co-authors have a prior relationship with Medtronic. Also, some of the study’s co-authors are current employees of Medtronic.
Read the full analysis from EuroIntervention here.