Cardiologists detail long-term outcomes of valve-in-valve TMVR
Valve-in-valve transcatheter mitral valve replacement (ViV TMVR) is associated with “little morbidity and low mortality” up to 13 years later, according to new research published in the Canadian Journal of Cardiology.[1] This represents the most detailed picture to date of the long-term outcomes of ViV TMVR.
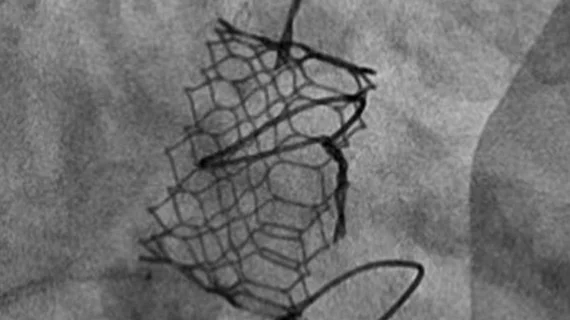
“ViV TMVR was first reported in 2009 using a transapical approach by our group,” wrote corresponding author John G. Webb, MD, an interventional cardiologist with the Centres for Heart Valve Innovation and for Cardiovascular Innovation and University of British Columbia, and colleagues. “Both transapical or transseptal TMVR have been shown to be a reasonable options for patients at high risk with redo mitral surgery. Favorable early outcomes have been reported and the number of implantations continues to grow worldwide. However, reports of long-term clinical and hemodynamic outcomes are lacking.”
The group examined data from a total of 119 ViV TMVR patients treated from 2008 to 2021. The mean patient age at baseline was 76.8 years old, and 55.4% of patients were women. The median time since each patient’s original mitral valve surgery was 9.8 years, and the study’s maximum follow-up period was 13.1 years.
The technical success rate was 97.5%. After 30 days, mortality was 2.5% and transcatheter heart valve (THV) thrombosis was seen in 2.5% of patients. One patient required a late THV balloon valvuloplasty for an elevated mitral valve gradient.
After one year, meanwhile, all-cause mortality was 10.1%. And after a median follow-up of 3.4 years, all-cause mortality jumped to 46.2%. Just 15.1% of those patients, however, died due to cardiovascular causes. Valve hemodynamics were “acceptable” after five years, the authors added.
After the study’s final follow-up period—13.1 years following the procedure for some patients—the authors noted that THV thrombosis was seen in 8.4% of patients, endocarditis was seen in 2.5% and structural valve dysfunction was seen in another 3%. Mitral valve reintervention had to be performed in 5% of patients, including redo ViV TMVR in 1.7% of patients.
“ViV TMVR can be performed with little morbidity and low mortality,” the authors wrote. “However, mid- to long-term survival remains limited in patients at high surgical risk due to comorbidities. Hemodynamic function is generally acceptable and structural valve dysfunction is infrequent in current high-risk patients. When structural THV dysfunction does occur, repeat ViV TMVR may be possible in selected patients.”
Comparing early patients vs. later patients highlights key improvements in valve-in-valve transcatheter mitral valve repair
The authors also examined outcomes for patients treated before and after 2016, when they started using the SAPIEN 3 THV and delivery system from Edwards Lifesciences, CT screening to anticipate left ventricle outflow tract obstructions and transseptal access as opposed to transapical access.
Fifty-seven percent of patients were treated after these changes were implemented, and those patients were associated with a higher technical success rate (100% vs. 94.1%), shorter median hospital stays (3 days vs. 7 days) and reduced 30-day mortality (1.5% vs. 3.9%). Five-year survival also improved, increasing from 41.1% to 74.7%.
“This likely reflects improved patient screening, improved THV devices, increasing experience, and technical improvements,” the authors wrote.
Read the full study here.