New 3D-printing technique shows early potential to help heart patients
Engineers have developed a new printing method using ink that solidifies when it interacts with ultrasound waves. The technique, deep-penetrating acoustic volumetric printing (DVAP), allows clinicians to 3D print structures inside the human body.
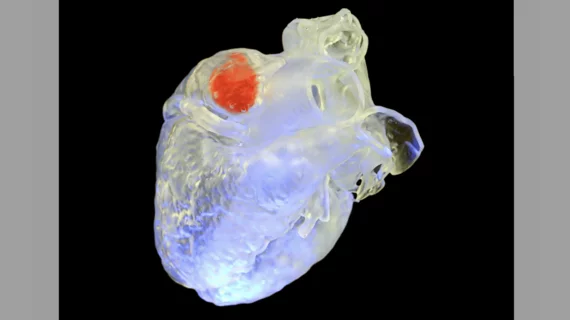
During DVAP, clinicians inject the ink deep under a patient’s skin and tissues—it is then targeted by ultrasound waves that cause it to solidify and form the desired shape. Early evidence suggests DVAP could be used to perform left atrial appendage closure (LAAC) and other important procedures in the not-so-distant future.
Y. Shrike Zhang, PhD, an associate bioengineer at Brigham and Women’s Hospital and associate professor at Harvard Medical School, and Junjie Yao, PhD, associate professor of biomedical engineering at Duke University, led the development of DVAP. The group shared its findings in Science.[1]
“DVAP relies on the sonothermal effect, which occurs when soundwaves are absorbed and increase the temperature to harden our ink,” Yao said in a prepared statement. “Ultrasound waves can penetrate more than 100 times deeper than light while still spatially confined, so we can reach tissues, bones and organs with high spatial precision that haven’t been reachable with light-based printing methods.”
“The ink itself is a viscous liquid, so it can be injected into a targeted area fairly easily, and as you move the ultrasound printing probe around, the materials in the ink will link together and harden,” added Zhang. “Once it’s done, you can remove any remaining ink that isn’t solidified via a syringe.”
One of the primary tests Zhang, Yao and the rest of their team performed was an LAAC on a goat. Once the DVAP process was complete, the group confirmed that simulated beating of the goat’s heart did not cause the 3D-printed part to break or come loose. Other tests included drug delivery in sample liver tissue and tissue reconstruction in a chicken. Both tests, like the LAAC procedure, appeared to be successful.
“We’re still far from bringing this tool into the clinic, but these tests reaffirmed the potential of this technology,” Zhang said.
“This work opens up an exciting new avenue in the 3D printing world, and we’re excited to explore the potential of this tool together,” added Yao.
Click here to read the full study in Science.