FDA grants new heart failure implant its breakthrough device designation
Restore Medical, an Israeli healthcare technology company focused on developing heart failure therapies, has received the FDA’s breakthrough device designation for its new ContraBand device. The designation specifically covers heart failure with reduced ejection fraction (HFrEF) patients with symptoms that persist even after undergoing guideline-directed medical therapy (GDMT). Patients should present without significant pulmonary hypertension or right heart failure to be considered for treatment.
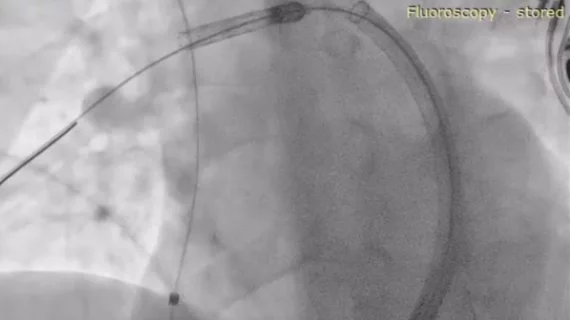
ContraBand is a transcatheter pulmonary artery banding system intended to improve the quality of life of patients presenting with persistent HFrEF. It is implanted through a minimally invasive procedure, leveraging the patient’s right ventricle to support their left ventricle.
The FDA’s decision was based in part on six-month and one-year results from a clinical trial exploring the potential safety and effectiveness of the ContraBand device. In March, Restore Medical shared an update on a first-in-human study of 15 heart failure patients treated with the device. All participants were already on GDMT, and they each experienced improved symptoms—including improvements in left ventricle ejection fraction—following treatment.
“The positive impact this treatment can have on the millions of people suffering from congestive heart failure cannot be underestimated,” Restore Medical CEO Gilad Marom, a veteran of the medical device industry, said in a 2021 statement. “Not only will it transform the quality of life of treated patients, but it will also reduce the enormous financial burden that comes as a result of patients being undertreated.”
What is the FDA’s breakthrough devices designation?
The FDA’s breakthrough devices program is designed to help medical devices make it through the approval process faster than they would otherwise. The agency’s representatives work directly with the device manufacturer, for example, and any submissions related to the device will be prioritized.