PCI before TAVR a winning combination for many heart patients
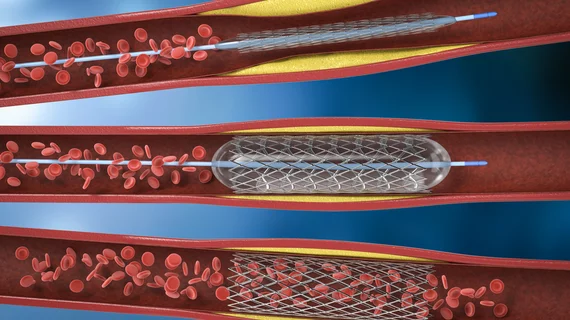
When patients present with coronary artery disease (CAD) and severe aortic stenosis (AS), performing percutaneous coronary intervention (PCI) prior to transcatheter aortic valve replacement (TAVR) is associated with better patient outcomes than addressing the CAD with a more conservative approach.
That was the key takeaway from NOTION-3, a new clinical trial presented at European Society of Cardiology (ESC) Congress 2024 in London and simultaneously published in The New England Journal of Medicine.[1]
“No clear recommendation currently exists in U.S. or European guidelines for performing PCI in addition to TAVR,” wrote first author Jacob Lønborg, MD, PhD, a cardiologist with Copenhagen University Hospital–Rigshospitalet, and colleagues. “The single randomized trial comparing PCI with conservative treatment in patients with coronary artery disease undergoing TAVR did not meet the requirement for noninferiority at one year and was terminated prematurely owing to futility, so no firm conclusion could be drawn.”
NOTION-3, sponsored by Boston Scientific, examined data from more than 400 patients who presented with stable CAD and symptomatic severe AS. All patients presented with at least one coronary stenosis with a fractional flow reserve (FFR) of 0.80 or less or a diameter stenosis of at least 90%.
The group was randomized to either undergo PCI or receive “conservative treatment” prior to TAVR from September 2017 to October 2022. The median patient age was 82 years old and median Society of Thoracic Surgeons score was 3%.
The conservative treatment consisted of a lifetime of daily aspirin therapy, and some patients were also prescribed daily clopidogrel for three months. Any additional treatment for this group was taken from modern CAD guidelines.
Overall, the study’s primary endpoint—a composite of all-cause mortality, myocardial infarction or urgent revascularization after two years—was seen in 26% of PCI patients and 36% of patients treated without PCI.
Bleeding events, however, were more common among PCI patients than those who did not undergo PCI (28% vs. 20%). In addition, 3% of patients in the PCI group had complication specifically related to revascularization.
“Our trial results suggest that PCI for lesions with an FFR of 0.80 or less or an angiographic coronary-artery diameter stenosis of at least 90% should be considered in all patients with severe AS undergoing TAVR,” the authors wrote. “However, the final decision to perform PCI should be individualized, with the patient’s age, overall health status and coexisting conditions, life expectancy, complexity and severity of the CAD, and bleeding risk all taken into account.”
While Boston Scientific did help fund this research, the company did not provide the authors with any devices or help in any way with performing the study or writing/editing the manuscript.
Click here to read the team’s full analysis.