Aortic valve calcium scores help predict need for a permanent pacemaker after TAVR
Aortic valve (AV) calcium scores may help cardiologists anticipate when patients face an increased risk of permanent pacemaker implantation (PPMI) after transcatheter aortic valve replacement (TAVR), according to new research published in Open Heart.[1]
“TAVR is increasingly used in the management of patients with severe aortic stenosis and has become the first-line treatment for patients over 75 years of age or at high surgical risk when femoral access is feasible,” wrote senior author Eric Durand, MD, an interventional cardiologist with the University of Rouen Normand in France, and colleagues. “Yet, its extension to younger patients is still limited by two main issues: the durability of percutaneous prosthesis, and the higher rate of PPMI compared with surgery. While the majority of complications have decreased over the past decade, the rate of PPMI remains high and, according to registries, has even tended to increase. Moreover, post-TAVR PPMI is associated with an increased risk of hospitalization for acute heart failure and mortality, thus leading to increased costs and resource utilization.”
AV calcium scores have previously been linked to predicting the presence of aortic stenosis and paravalvular leak. Durand et al. aimed to learn if those prognostic abilities carried over to PPMI after TAVR as well.
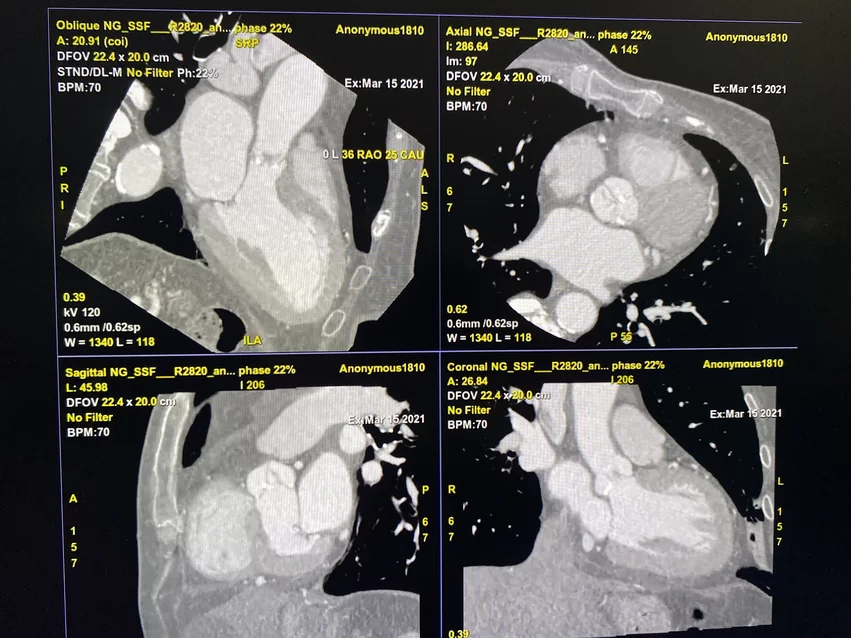
The group explored data from more than 700 TAVR patients treated at a single facility from 2016 to 2022. Only patients with available AV calcium scores obtained using CT imaging were included. The median age was 84 years old, 50% of patients were men and common comorbidities included hypertension, diabetes and coronary heart disease. While 24% of patients had undergone a previous percutaneous coronary intervention, another 3.8% had undergone a previous coronary artery bypass graft procedure.
Overall, 16% of TAVR patients required PPMI after 30-day follow-up. The median time of PPMI was two days after TAVR. The most common reasons patients required the pacemaker were high-degree atrioventricular (AV) block (68%), a high risk of complete AV block (28%) and sinus node dysfunction (4%).
Patients who required PPMI were more likely to be male then female. These patients were also more likely to present with first-degree AV block and right bundle branch block (RBBB) prior to treatment.
Durand et al. found that AV calcium scores were “significantly higher” in patients who required PPMI than those who did not. RBBB remains the single strongest predictor for PPMI after TAVR, they wrote, but high AV calcium scores showed potential to help identify patients at an increased risk, especially when combined with “other known traditional risk factors.”
“By better stratifying PPMI, we could direct patients towards shorter care pathways, thereby optimizing resource utilization,” the authors concluded. “Further studies are needed to confirm our results in a larger sample and in a multicenter study.”
Click here for the full analysis.