Atherectomy’s Small But Growing Presence
Throughout its nearly 30-year history, atherectomy has remained something of an under-achiever.
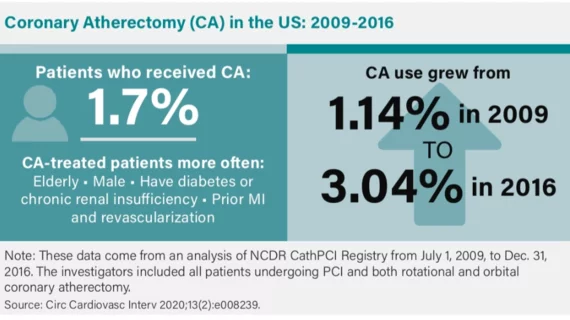
Witness a 2020 study in Circulation: Cardiovascular Interventions, where Ajay Kirtane, MD, SM, of Columbia University Medical Center, and co-authors found that adjunctive coronary atherectomy was performed in just 3 percent of the nearly four million cases drawn from the CathPCI Registry in the fourth quarter of 2016, up from 1.1 percent in the third quarter of 2009. The study also revealed that nearly 35 percent of hospitals that offered PCI didn’t perform coronary atherectomy at all. The authors further found that increasing hospital coronary atherectomy volume was linked to a 15 lower risk percent of mortality and 33 percent lower risk of PCI failure or complications requiring CABG (2020;13[2]:e008239).
OVERDUE FOR A SURGE?
Why, then, is atherectomy so rarely deployed, particularly in light of the surge of coronary calcification?
The technology has hardly remained static. Rotational atherectomy began to gain traction in 1993 when Boston Scientific received FDA approval for Rotablator. With the introduction of stenting shortly afterwards, the device took on an adjunctive role for plaque modification in moderately to severely calcified obstructions. The roll-out of orbital atherectomy in 2013 with the Diamondback 360 (Cardiovascular Systems) served to expand the overall market for these high-speed tools that, unlike IVL, grind their way through arterial vessels, abrading hard tissue into small particles. Refinements to existing devices (like Rotapro in 2019, the first new version of Rotablator in over two decades), and other technologies about to undergo studies hint at the growth potential for these workhorse devices that sand, cut, shave or vaporize plaque in order to better prepare vessels for stenting.
Kirtane’s study on coronary atherectomy weighed the advantages (better lesion preparation, improved stent delivery, expansion and apposition) against the disadvantages (prolonged procedural times, slow or no-reflow, coronary perforation and increased cost), but reached no firm conclusion about its tepid clinical deployment.
“It could be training issues or concerns over safety due to unfamiliarity with these devices,” Kirtane suggests. “But I personally believe that dedicated calcium modification strategies such as atherectomy are underutilized today. This is the primary reason we’re doing the ECLIPSE [Evaluation of Treatment Strategies for Severe Calcific Coronary Arteries: Orbital Atherectomy vs. Conventional Angioplasty Technique Before Implantation of Drug-eluting Stents] trial, randomizing 2,000 patients to an orbital atherectomy-based strategy vs. a conventional balloon angioplasty strategy for treating severely calcified lesions prior to the implantation of drug-eluting stents.”
Diamondback 360, with its orbiting diamond-covered crown on a special delivery wire, has helped to move the needle for atherectomy. Compared to rotational, orbital atherectomy “is a slightly more user-friendly device with easier set-up, and it theoretically allows for continued blood flow to occur during the ablating part of the process,” notes Savage. “People like these aspects of orbital atherectomy even though it involves a bigger expense than rotational.”
A study comparing rotational atherectomy with orbital atherectomy found the latter was associated with a lower risk of significant dissection, but that the rates of perforation, bleeding, stent thrombosis, emergency or salvage CABG and all-cause death were similar (J Am Coll Cardiol 2019;74[13]:Suppl B25). The study’s verdict: Rotational atherectomy and orbital atherectomy “have comparable safety and effectiveness in facilitating PCI in heavily calcified coronary lesions.”
In an editorial accompanying Kirtane’s Circulation: Cardiovascular Interventions study, Shing-Chui Wong, MD, from New York-Presbyterian, cited the importance of both ablative tools. “The lesion modification rendered by [coronary atherectomy] certainly eases equipment delivery and optimizes stent expansion. This study emphasizes the importance of familiarity with all devices old and new in the catheterization laboratory. This is a responsibility not only of the operators but also the institution support team.”
Even with refinements, though, atherectomy faces continued challenges to its mainstream acceptability. “Atherectomy is a modality that’s used in a minority of cases,” acknowledges Chandan Devireddy, MD, associate professor medicine at Emory University in Atlanta and a site investigator for DISRUPT CAD III who has done consulting for Shockwave. “The issue with atherectomy is that you’re cutting calcified plaque at very high speeds, which then has to be absorbed by the body, and always in the back of your mind are concerns of embolization, dissection or clinical instability. Lithotripsy, on the other hand, might offer a straight-forward, low-pressure treatment with soundwave energy. The amount of change that occurs in calcified tissue after treatment with one balloon seems to be impressive based on what I’ve seen and the results of early clinical trials.”