Rebounding & Rebooting: Tips & Tactics for Cardiology Practices
Tips & Tactics for Cardiology Practices
As COVID-19 ebbs and flows and cardiologists strive to recover from the tests and procedures lost during shutdown, the onus is on healthcare teams to deliver creative strategies to bring back apprehensive patients while safely and effectively managing readjusted workflows and protocols.
More alarming than the huge financial hit that cardiology practices have seen is that too many patients with urgent conditions weren’t seeking treatment. CDC statistics show that in the 10 weeks following the March 13 declaration of the COVID-19 national emergency, trips to the hospital fell 23% for heart attacks and 20% for stroke. “People were having heart attacks and being found dead in their homes,” says Christopher J. White, MD, professor and chair of Medicine and Cardiology at Ochsner Medical Center in New Orleans. “That was a clear sign to us they were avoiding the hospital.”
White and other voices in cardiology offered thoughts and suggestions on how CV practices can fuel recovery by retooling in practical and proven ways.
“We went through every patient on our 90-day rolling schedule of planned visits and called them all to make sure we weren’t losing anyone. ... We prioritized staying connected.” Christopher J. White, MD Ochsner Medical Center, New Orleans
ORGANIZE & PRIORITIZE
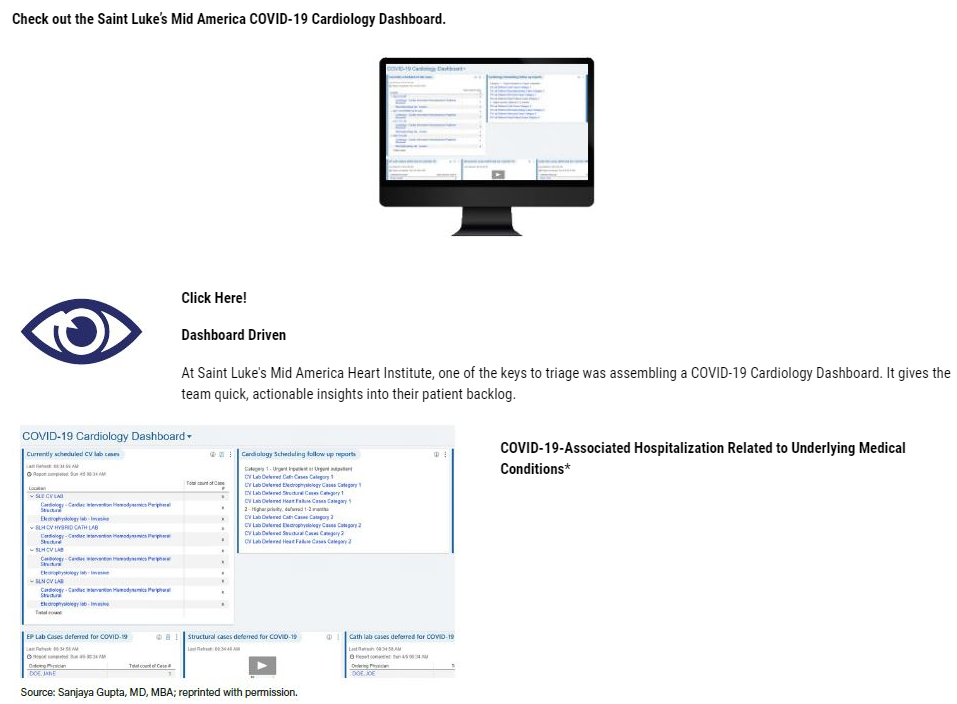
At the outset of the COVID-19 crisis, Saint Luke’s Mid America Heart Institute in Kansas City saw the need to convert to a more virtual workflow in its cardiology group practice. The group formed a team of specialists from electrophysiology, interventional cardiology and cardiac surgery to develop a four-step system for classifying a growing backlog of patients for treatment: 1) Urgent Inpatient or Urgent Outpatient, such as unstable angina; 2) Higher Priority, such as stable angina with 15% ischemia, for scheduling within one to two months; 3) Lower Priority, such as stable claudication and stenting, to be done within two to three months; and 4) Elective, such as PFO closures, that could be deferred four to six months.
“By carefully triaging patients with the greatest need while deferring those who could be safely stabilized and postponed, we were able to return to above full capacity within a few weeks,” explains Sanjaya Gupta, MD, MBA, an electrophysiologist at Saint Luke’s Mid America and assistant professor of medicine at the University of Missouri-Kansas City. Critical to that process was the creation of a COVID-19 Cardiology Dashboard, which enabled clinic supervisors and administrators to get a quick fix on how many patients were waiting in the queue for Urgent and Higher Priority procedures as well as for tests. “We had it organized so things never got out of control,” Gupta says.

“By carefully triaging patients with the greatest need while deferring those who could be safely stabilized and postponed, we were able to return to above full capacity within a few weeks.” Sanjaya Gupta, MD, MBA, Saint Luke’s Mid America Heart Institute, Kansas City, Mo.
RECAPTURE LOST BUSINESS
After months-long lockdowns of many cardiovascular outpatient practices and clinics earlier this year, working amidst COVID-19 has meant aggressively mobilizing systems, strategies and personnel to recapture lost business. In New Orleans, Ochsner Medical Center’s cardiac clinic deployed its RNs and medical assistants to comb through the medical records to determine, in consultation with physicians, which patients needed to come in immediately and which could wait. “We went through every patient on our 90-day rolling schedule of planned visits and called them all to make sure we weren’t losing anyone,” recalls White. “We’re now running at 118% of our planned capacity.”
Helping Ochsner reduce the backlog was an extension of its outpatient clinic hours on weekdays and weekends. Part of their strategy was overbooking—in fact, nearly doubling—the number of patients slotted into its block schedule knowing that a certain percentage would opt for televisits instead of coming onsite. “We prioritized staying connected,” White explains.
MAKE TELEHEALTH WORK
Video and telephone visits with doctors became the lifeline that kept many cardiology practices afloat in the midst of the public health emergency. Saint Luke’s Mid America converted nearly 450 established or annual patients to the virtual platform within the first three days of its transition plan, with new and consult patients added shortly thereafter.
While most clinicians believe telemedicine is here to stay, given the need for social distancing and patients’ affinity for convenience, there is also a strong belief that telehealth is not about to replace face-to-face visits. “We’re seeing that telehealth is often not the preferred vehicle, that our patients actually want to come back into the office,” observes Cathie Biga, MSN, RN, president and CEO of Cardiovascular Management of Illinois.
For cardiology practices, the happy medium is a work in progress where nonemergent patients are given options. Though Saint Luke’s Mid America has transitioned back to seeing patients in the office, they still offer video visits, “particularly for the elderly who have transportation issues or are concerned about in-office exposure,” says Gupta.
AVOID ‘ANALYSIS PARALYSIS’
In times of crisis, nothing is more important than speed to execution, cardiologists told CVB. The key to survival can be your ability to quickly assess the problem and its solutions, and then take decisive action. Too often, however, healthcare falls into overthinking to the point where movement slows to a painful crawl. Biga calls this common trap “analysis paralysis.”

The antidote? “Don’t worry about poring over every little detail,” Biga advises. “There is plenty of great COVID-19 guidance ... in areas like triage, reopening imaging and non-COVID care, assessing the workplace risk of COVID-19 for cardiac patients, and keeping your staff safe. Let’s draw on information like that and not spend the next month trying to figure it all out.”
Cardiology practices have taken a big financial hit. Their bounce-back pace varies depending on a number of factors, such as early COVID-19 penetration, degree of resurgence, practice size and resilience.
- Rebound speed also can be impacted by the strategies teams use during these challenging times. Get creative, experts told CVB, and ramp up communications with fearful patients and their families.
- Get organized ASAP. By leveraging the talents and tools available, you can set up systems to help you track patient backlog, prioritize cases and connect with patients on the platform they prefer.
- Right-size telehealth for your practice. Telehealth works really well for some patients and procedures. For others, it’s a backup plan.
- Keep moving forward. Don’t get so caught up in assessing options that you lose sight of your patients’ needs or the health of your practice.
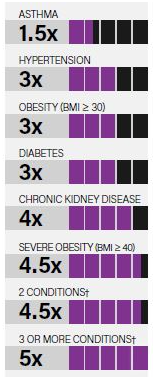
Source: CDC.gov, citing Ko JY, Danielson ML, Town M et al. 2020. Accessed Aug. 28, 2020 at https://www.cdc.gov/coronavirus/2019-ncov
Notes
*Compared to patients without the conditions.
**Conditions include asthma, obesity, diabetes, chronic kidney disease, severe obesity, coronary artery disease, history of stroke and COPD. Source: CDC. gov, citing Ko JY, Danielson ML, Town M et al. 2020. Accessed Aug. 13, 2020, at CDC.gov https://www.cdc.gov/coronavirus/2019-ncov
PULSE POINT
MEDICAL GROUPS HURTING
NEARLY 40% of surveyed medical groups say their monthly revenue has been halved, or worse.
MORE THAN 90% of medical groups forecasted increased PPE and telehealth infrastructure costs.
TOP TRENDS TO WATCH*
A new Definitive Healthcare report revealed trends that healthcare leaders think will have the greatest impact on the industry in the year ahead.
1. Hospitals’ revenue loss due to delayed or reprioritized elective surgeries
2. Consequences of delayed care
PHYSICIANS SAY...
49 % of surveyed U.S. physicians believe the pandemic will not be under control until **after June 1, 2021.**1
N=3,513 responses
- Source: The Physicians Foundation. 2020 Survey of America’s Physicians: COVID-19 Impact Edition. https://physiciansfoundation.org/research-insights/2020physiciansurvey/
- Accessed Sept. 1, 2020, at . 2. Source: Definitive Healthcare. 2020 Trend Report: Predicting COVID-19’s Long-Term Effects. Accessed Sept. 1, 2020, at .
https://www.definitivehc.com/resources/healthcare-insights/predicting-covid-19-long-term-effects - 3. Source: AMGA. (June 16, 2020). "Medical Groups and Integrated Health Systems Still Experiencing Significant Revenue Losses; Many Providers Forecast at Least a Year Until Revenues Return to PreCOVID Levels." Accessed Sept. 1, 2020, at .
https://www.amga.org/about-amga/amga-newsroom/press-releases/release-on-may-survey/
