3D echo comparable to CT for predicting TMVR complications
Cardiologists may be able to use echocardiography instead of cardiac CT to predict the risk of left ventricular outflow tract (LVOT) obstruction prior to transcatheter mitral valve replacement (TMVR), according to new data published in JACC: Cardiovascular Imaging.[1]
LVOT obstruction after TMVR remains a significant concern among structural heart cardiologists. Predicting the risk of LVOT obstruction typically requires CT, which comes with certain disadvantages compared to other imaging options.
The study’s authors—including first author Joanna Bartkowiak, MD, an interventional cardiologist with New York-Presbyterian/Columbia University Irving Medical Center (NYP/CUIMC), and senior author Rebecca T. Hahn, MD, a professor of medicine with NYP/CUIMC and director of interventional echocardiography at the Columbia Structural Heart and Valve Center—examined the potential value of using 3D transesophageal echocardiography (TEE) instead of CT to anticipate the risk of LVOT obstruction prior to TMVR. TEE is performed on all patients screened for TMVR; this makes it a sensible alternative to CT, which may not be otherwise required in some patients.
The group retrospectively examined data from 105 consecutive patients who underwent TMVR at one of two tertiary care centers from October 2017 and May 2023. The mean age was 75.8 years old, and 56% of patients were male.
The cohort included patients who underwent TMVR with dedicated mitral valve bioprostheses in addition to those treated with aortic transcatheter valve bioprostheses for a degenerative surgical valve (valve-in-valve TMVR), degenerative annuloplasty ring (valve-in-ring TMVR) or native valve–in–mitral annular calcification (ViMAC TMVR).
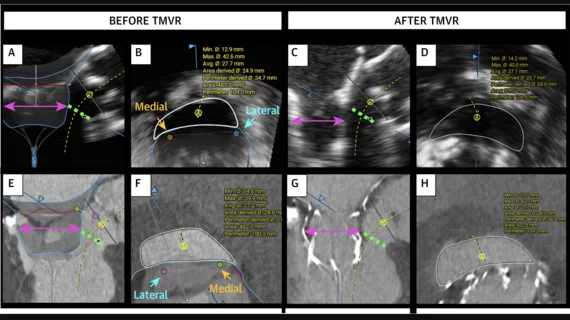
A virtual valve was projected onto the baseline CT and 3D TEE images of each patient, and then mitral annular (MA) and neo-LVOT dimensions were measured in scans taken before and after the TMVR procedures. Researchers then compared all measurements to baseline CT imaging results, and predicted LVOT measurements were compared with the actual postprocedural measurements.
Overall, neo-LVOT measurements obtained using 3D TEE were comparable to results obtained using CT. The two measurements delivered similar accuracy, though 3D TEE did tend to underestimate MA dimensions in patients who presented with native mitral valve disease.
“The underestimation may be related to acoustic ‘noise’ or ‘blooming artifact’ which could be improved by reducing the gain,” the authors wrote. “Although the mean differences may not inherently hold clinical significance, wide limits of agreement for MA area suggest that TEE and CT assessment could lead to different device sizing. This is less of a concern in valve-in-valve and valve-in-ring cases because the valve choice is based on the true size of surgical implant and online-application recommendations.”
The group also highlighted the similarity between 3D TEE and CT when it came to anticipating LVOT gradient increases.
“Other determinants of gradients besides neo-LVOT area are left ventricle contractility and loading conditions,” the authors wrote. “Additionally, in the whole population, only seven patients had a gradient increase of more than 30 mm Hg and three were excluded from the correlation analysis because of the anterior leaflet laceration performed before the implantation. Nevertheless, the predicted neo-LVOT area continues to be the most reliable predictor of LVOT obstruction and the correlation of this parameter with gradients remained consistent across both imaging modalities.”
More research is still needed to determine if 3D TEE can consistently deliver pre-TMVR measurements comparable to CT. Bartkowiak et al. called for a prospective, multicenter study to confirm their findings.
Read the full analysis here.