Targeting the left atrial posterior wall (LAPW) when patients with persistent atrial fibrillation (AFib) undergo pulsed field ablation (PFA) does not significantly improve outcomes, according to new research presented at AF Symposium 2024 in Boston. The findings were simultaneously published in JACC: Clinical Electrophysiology.[1]
“Pulmonary vein isolation (PVI) is the cornerstone of catheter ablation therapy for AFib,” wrote first author Mohit Turagam, MD, an electrophysiologist and associate professor of medicine with the Icahn School of Medicine at Mount Sinai, and colleagues. “While the PVI-only approach to ablation for paroxysmal AFib has improved in the last decade, the clinical success rates in patients with persistent AFib have remained suboptimal, with single-procedure success ranging from 43% to 67%. In an attempt to improve outcomes, adjunctive strategies targeting AFib sources (e.g., non–pulmonary vein triggers) and empiric atrial substrate modification have been pursued—including ablation of the left atrial posterior wall (LAPW), mitral isthmus, left atrial appendage, low voltage areas and complex fractionated atrial electrograms.”
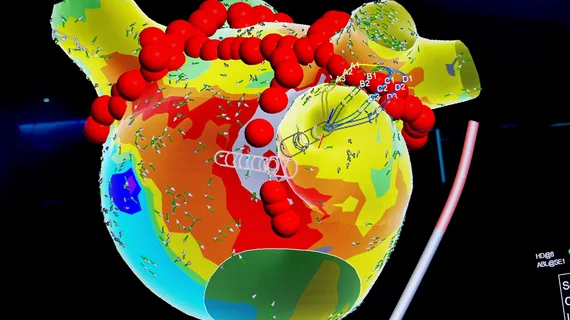
The LAPW represents a potential target during PFA, the authors explained, due to its “embryological origins from the pulmonary veins, complex architecture and propensity for fibrosis-related conduction delay.” To investigate this potential, the group explored data from more than 500 patients with persistent AFib who underwent PFA in Europe from March 2021 to May 2022. While 76% of those patients underwent just PVI ablation, the other 24% were treated with PVI in addition to LAPW ablation.
Overall, 66.4% of patients who underwent both types of ablation did not have recurring AFib 12 months after the procedure; this was comparable to the 73.1% of patients who did not have recurring AFib 12 months after undergoing PVI ablation alone.
Major adverse events, meanwhile, were seen in 2.2% of patients who underwent PVI and LAPW ablation and 1.4% of patients who only underwent PVI ablation.
These comparable outcomes, despite additional treatment, ultimately suggest that it was not beneficial to treat these patients with LAPW ablation.
"The study's cautionary note about not performing empiric left atrial posterior wall ablation as a purely anatomical approach for persistent AFib suggests a need for a more thoughtful and selective approach,” Turagam said in a statement from Mount Sinai.
Pulsed field ablation gaining momentum
PFA continues to gain momentum in the United States, with both Medtronic’s PulseSelect and Boston Scientific’s Farapulse gaining U.S. Food and Drug Administration (FDA) approval in recent months. Other vendors such as Abbott are also actively working toward securing key regulatory approvals, a sign that the entire electrophysiology space understands the importance of this trend.
Because it uses electric pulses as opposed to extreme temperatures, limiting the risk of harmful complications, PFA may go on to become the go-to treatment option over radiofrequency or cryoballoon ablation when AFib patients require care.