FAI helps quantify vascular inflammation, predict future CVD events in cardiac imaging patients
The addition of perivascular fat attenuation to routine coronary computed tomography angiography (CTA) improves risk stratification in heart patients, according to research presented at the European Society of Cardiology (ESC) annual symposium in Munich, surpassing current prognostic models to re-classify and predict cardiac deaths with more accuracy.
“Coronary CTA is a sensitive and widely used non-invasive imaging modality for diagnosing coronary artery disease,” lead investigator Evangelos K. Oikonomou, MD, of the Radcliffe Department of Medicine at the University of Oxford in the U.K., and colleagues wrote in a study published simultaneously in the Lancet. “It is also used for diagnosis and management of chest pain. However, coronary CTA focuses predominantly on identification of anatomically significant coronary artery stenosis, which is seen in fewer than 50 percent of patients referred for this test.”
What’s more, Oikonomou and co-authors said, the majority of acute coronary syndromes stem from unstable but non-obstructive atherosclerotic plaques, which aren’t easily identified with today’s non-invasive imaging tools. It’s also difficult to capture vascular inflammation, a driver of atherosclerotic plaque formation.
“Currently, no method is readily available to allow early detection of vascular inflammation in coronary arteries,” the researchers wrote. “Such a method would enable timely deployment of measures to prevent disease development and future heart attacks.”
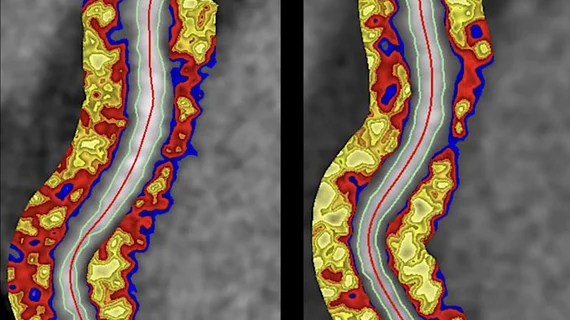
Since coronary artery inflammation inhibits the accumulation of fats and adipocyte differentiation in adjacent perivascular fat, Oikonomou et al. turned to an imaging biomarker known as the perivascular fat attenuation index, or the FAI. Since the FAI can detect and quantify coronary inflammation, the authors said they could use that data to predict future adverse events.
The team conducted a post-hoc analysis of outcome data gathered prospectively from two independent cohorts of patients undergoing coronary CTA — one group of 1,872 in Erlangen, Germany, and one of 2,040 in Cleveland, Ohio. After an average six years of follow-up, they found high perivascular FAI values around the proximal right coronary artery and left anterior descending artery were predictive of all-cause and cardiac death in both cohorts.
“Therefore, the perivascular FAI measured around the right coronary artery was used as a representative biomarker of global coronary inflammation,” Oikonomou and colleagues said. “FAI improved risk discrimination in both cohorts, leading to significant reclassification for all-cause and cardiac mortality.”
The researchers said they calculated the optimum cutoff for perivascular FAI at -70 • 1 Hounsfield units, above which point patients would likely see a steep increase in cardiovascular mortality.
In a related Lancet editorial, Amir A. Mahabadi and Tienush Rassaf, both of the Department of Cardiology and Vascular Medicine at University Hospital Essen in Germany, said despite the strengths of Oikonomou and colleagues’ study, measuring perivascular FAI is “relatively time-consuming” and restricted to practices with the expertise to do so.
“This complexity necessitates automated software programs, enabling quick and reliable quantification of the perivascular FAI to allow its implementation in everyday clinical routine,” Mahabadi and Rassaf said. “If these obstacles are resolved, characterization of atherosclerosis could have a role in preventive cardiology.”
Related Cardiac CT Content:
VIDEO: Office-based cardiac CT and FFR-CT offer a new business model
Imaging group says new guidelines for chest pain contain some ‘troubling recommendations’
American Society of Nuclear Cardiology says AHA/ACC chest pain guidelines miss the mark
Expert panel recommends coronary CTA as first choice when evaluating for stable CAD
VIDEO: Use of CT to assess coronary plaques
VIDEO: Example of photo-counting cardiac CT with calcified coronaries
VIDEO: HeartFlow FFR-CT sees increased interest after inclusion in the 2021 Chest Pain Guidelines
Statin reduces risk for non-obstructive CAD patients but no significant risk reduction for aspirin