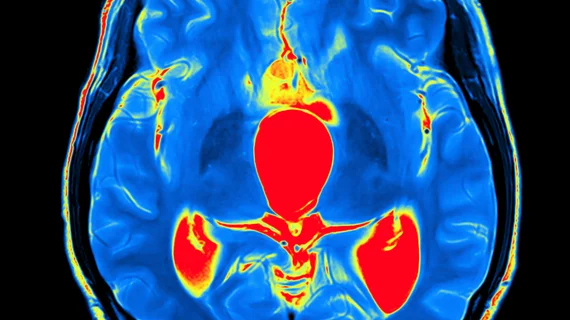
Brain MR imaging linked to better outcomes for patients with acute ischemic stroke
Using brain MR imaging to evaluate patients with acute ischemic stroke is associated with improved in-hospital outcomes, according to a new study published in the Journal of the American Heart Association.
Researchers explored the National Inpatient Sample (NIS) database, reviewing the outcomes of more than 94,000 adult patients who underwent a brain MRI for acute ischemic stroke from 2012 to 2014. The team then make comparisons using a control group of more than 1.5 million patients from the same database.
Overall, the use of brain MRI was associated with a steady reduction in in-patient mortality (1.67% vs 3.09%). It was also linked to “significantly lower incidence” of both gastrostomy and mechanical ventilation, though there was no significant difference in intracranial hemorrhage between the two groups.
The study’s authors did note that brain MRI uses more resources, with lengths of stay increasing by 8% and total costs increasing by 11%. Considering the key benefits also identified, however, these changes were described as “marginal.”
“The clinical benefits associated with inpatient brain MRI outweigh the resource requirements,” wrote lead author Hwan Lee, MD, department of radiology at the Pennsylvania Perelman School of Medicine in Philadelphia, and colleagues. “The present study provides the first evidence for the relationship between inpatient brain MRI and in‐hospital outcomes in acute ischemic stroke. A prospective, randomized study is needed to establish causality and to characterize the change in patient management following inpatient brain MRI.”
The study did have certain limitations, the team added. For example, relying on data taken from the NIS database makes it difficult to reach certain conclusions.
“Lack of information on the clinical context of receiving MRI is an intrinsic limitation of the NIS database, and it prohibits making any conclusions on causation from our study,” the authors wrote. “Similarly, the lack of information on detailed patient management in the NIS database precluded characterization of the change in management associated with brain MRI.”