MRI-based small vessel disease score linked to future stroke, dementia
A simple score containing four MRI markers of cerebral small vessel disease (CSVD) is associated with stroke, dementia and mortality among older adults, according to an analysis of the population-based Rotterdam Study published Oct. 24 in Stroke.
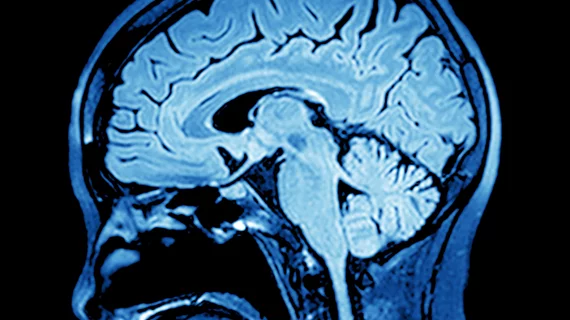
The study included 1,651 participants—73.3 years old on average; 54.5 percent women—who had no history of stroke or dementia at baseline. All patients underwent brain MRI with 1.5 Tesla scanners, and the images were used to calculate a CSVD sum score from 0-4 based on the following characteristics: white matter hyperintensities (WMH), lacunes, cerebral microbleeds and perivascular spaces (PVS).
One point was added to the score if a patient’s WMH volume fell in the third or fourth quartiles, if a patient had at least one lacune (subcortical lesion between 3 and 15 millimeters), at least one microbleed or had 11 or more perivascular spaces between 1 and 3 mm.
Previous studies focused on the application of the sum score to predict general cognitive function, vascular risk factors and gait and balance, but the authors suggested the practical use of the score would increase greatly if it were also predictive of harder clinical endpoints like stroke, dementia and mortality.
And in this population, each one-point increase in the CSVD score was linked to a 54 percent increased risk of stroke, 25 percent increased risk of dementia and 15 percent risk of increased mortality at 10 years, after adjustment for age, sex and clinical characteristics included in the Framingham Stroke Risk Profile.
“In a community-dwelling population, a higher CSVD score on MRI shows stronger associations with risk of stroke, dementia, and mortality than individual markers,” wrote lead author Pinar Yilmaz, MD, MSc, with Erasmus Medical Center in Rotterdam, the Netherlands, and colleagues. “This suggests that the score better reflects the global measure of CSVD-related brain damage. Future research should explore improving knowledge of CSVD pathology with advanced imaging markers and subclinical detection to stratify high-risk individuals for CSVD.”
Yilmaz et al. noted their study was the first to use automated volumetry for WMH in the sum score, which they believe could improve the practicality and efficiency of measuring that marker.
“Another CSVD feature that could greatly benefit from quantification is PVS ratings because the count for these is time consuming and prone to observer variability,” they wrote. “Yet, to date, no automated algorithms are available. New imaging biomarkers could be other volumetric measurements, white matter microstructure, and microinfarcts.”
The use of 3T MRI scanners also has the potential to detect small vessel disease markers with more sensitivity, the researchers pointed out, which could affect the CSVD score. However, the 1.5T scanners used in this study were consistent with previous studies of the sum score.
Yilmaz and colleagues said most of the associations between the clinical outcomes and individual MRI markers—and even the combined sum score at low values—were statistically insignificant. But they attributed this to low event rates during the average follow-up of 7.2 years; 66 patients had strokes, 76 developed dementia and 306 died. Even if statistically insignificant from one value to the next, the hazard ratio for all of the outcomes increased incrementally with higher CSVD sum scores compared to a score of 0.
The authors said scoring each MRI marker as a 0 or 1 based on specific cutoff criteria might sacrifice the power of nuanced information, but is likely more applicable in a practical clinical setting. Another limitation of the study was its predominantly white patient cohort, which may limit generalizability to other populations.