New cardiac imaging strategy could reduce ICA, PCI rates
Using artificial intelligence (AI) software to evaluate coronary CT angiography (CCTA) exams may help reduce the use of invasive coronary angiography (ICA) and percutaneous coronary intervention (PCI), according to new research published in Radiology: Cardiothoracic Imaging.[1]
A large academic medical center performed a retrospective analysis of data from nearly 3,000 patients who underwent CCTA without heart rate control from August 2020 to August 2021. The most common reason for the initial CCTA referral was angina. The group’s goal was to assess how referring some patients for assessment with HeartFlow’s FFRCT Analysis technology, which uses AI to evaluate CCTA results for warning signs of CAD, could potentially impact patient care.
Overall, 9.7% of patients were chosen to undergo assessment with the HeartFlow software, which delivered CT-derived fractional flow reserve (CT-FFR) results for each patient. The “selective use” of this technology helped keep costs down for patients who were much less likely to benefit from the additional evaluation. Nearly three in four patients chosen for this treatment presented with CAD-RADS category 3 lesions.
“In patients with moderate narrowing or blockage of the arteries, there can be ambiguity about who would benefit from invasive testing and revascularization procedures,” Mangun Kaur Randhawa, MD, a post-doctoral research fellow with the Massachusetts General Hospital (MGH) department of radiology, said in a statement. “CT-FFR helps us identify and select those patients who are most likely to benefit.”
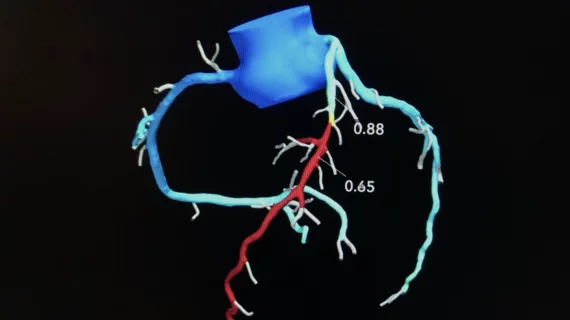
A negative CT-FFR result was seen as anything higher than 0.80, a positive result was anything 0.75 or lower and a “borderline” result was anything from 0.76 to 0.80. Randhawa et al. found that 56.3% of patients selected to undergo treatment with the HeartFlow offering had a negative result, 30.9% had a positive result and 12.6% had a borderline result.
Importantly, patients with significant narrowing of the arteries who underwent CT-FFR had much lower rates of ICA (25.5% vs. 74.5%) and PCI (21.1% vs. 78.9%) in the subsequent three months than patients who did not undergo CT-FFR. Also, positive CT-FFR results were associated with higher odds of still requiring ICA or PCI during that three-month window. These findings, the authors explained, suggests that using CT-FFR on a case-by-case basis can help care teams limit the use of ICA and PCI in patients who present with angina or other symptoms of suspected coronary artery disease.
“CT-FFR helps us identify patients who would most benefit from undergoing invasive procedures and to defer stenting or surgical treatment in patients who likely won’t,” senior author Brian B. Ghoshhajra, MD, associate chair for operations and academic chief of cardiovascular imaging at MGH, added in the same statement. “CT-FFR makes the CT ‘better’, but we found that the benefits were highest when used selectively.”
Click here to read the full study in Radiology: Cardiothoracic Imaging.