Plaque characteristics boost predictive power of CTA risk scoring
A CT angiography (CTA)-derived score that also incorporated the extent, location and composition of coronary plaque outperformed a model that focused only on the severity of stenosis, researchers reported Jan. 16 in JACC: Cardiovascular Imaging.
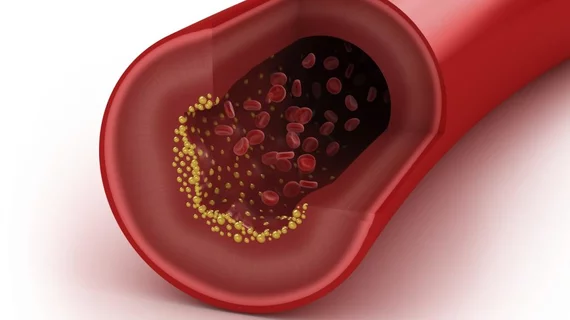
Coronary CTA reading is currently guided by the Coronary Artery Disease-Reporting and Data system (CAD-RADS), and that assessment is predicated mostly on the maximal degree of stenosis observed. However, lead author Alexander R. van Rosendael, MD, and colleagues noted that other coronary plaque characteristics including its location (proximal versus distal), composition (calcified, noncalcified or mixed) and the number of plaques have been linked to clinical outcomes in previous studies.
“The integration of this complex information into a risk score may further optimize risk stratification and enable maximum use of information derived from coronary CTA,” van Rosendael, with Leiden University Medical Center in the Netherlands, and co-authors wrote.
To test this theory, the researchers used their new comprehensive CTA score in a cohort of 2,134 patients with suspected coronary artery disease and evaluated its ability to predict the composite endpoint of myocardial infarction or death.
Overall, the new score was a better predictor of those events over an average follow-up of 3.6 years, achieving a c-statistic of 0.768 when added to seven commonly collected clinical variables. The c-statistic was 0.742 for the CAD-RADS model plus those variables.
In addition, the comprehensive score showed a net reclassification improvement of 12.4 percent in terms of shifting patients between low-, intermediate- and high-risk groups.
“The current study has shown the improved prognostic significance of a comprehensive CTA score incorporating multiple aspects of plaque detected by coronary CTA (plaque extent, severity, location, and composition) to predict major clinical outcomes,” van Rosendael et al. wrote. “Compared with the CAD-RADS, our new comprehensive score provided improved prediction of outcomes and reclassification of risk for future events.”
The authors also tested their model in an external validation cohort of 1,971 patients with a mean 5.2 years of follow-up, finding it again outperformed the CAD-RADS (c-index: 0.718 versus 0.689).
The comprehensive CTA score includes a 17-segment model of the coronary artery tree based on American Heart Association criteria; uses the Leaman score to provide weight factors for plaque location; and draws from previous literature on the predictive values of plaque extent, severity and composition. When no plaque is present, the score for that segment is zero. However, when plaque is observed the modifying factors of plaque location, plaque composition and stenosis severity are multiplied together according to prespecified weights to determine the score for that particular segment.
A link to the risk score calculator, which produces a result from 0 to 42 after summing all segment scores, is available here.
“The new score may be used to tailor medical treatment to the individual patient by maximizing therapy for patients in the highest risk group: targeting of very low cholesterol levels and optimizing blood pressure, and possibly reduce therapy for patients in the lowest risk group to minimize side effects of medication,” the researchers wrote. “Future studies should investigate whether clinical outcomes can be improved by the clinical application of this approach of personalizing risk stratification.”
Including these plaque characteristics makes the score more complicated to calculate, the authors acknowledged, although they said automated calculation is “feasible.”
Writing in a related editorial, Belgian cardiologists Carlos Collet, MD, and Martin Penicka, MD, PhD, said other limitations of the study must also be considered.
“Although the investigators claimed a superior risk discrimination compared with the established CAD-RADS system, the analysis was biased in favor of the new score because it did not incorporate plaque information in the CAD-RADS score,” Collet and Penicka wrote. “Adverse plaque features (e.g., positive remodeling and low attenuation plaque) are modifiers of the CAD-RADS score and may prompt physicians to initiate or intensify medical therapy.”
Both van Rosendael et al. and the editorialists agreed that incorporating functional assessments of stenosis—for instance, with fractional flow reserve—could further improve risk prediction and deserves to be investigated.
Ultimately, Collet and Penicka believe developments in artificial intelligence will drive the most effective applications of these imaging techniques.
“Feeding machine learning algorithms with comprehensive coronary CTA evaluations may enhance the quest for the vulnerable patient and has the potential to better discriminate risk and tailor therapy,” they wrote. “The work of van Rosendael et al. is a step forward in this direction.
“Advancements in the field, such as the automatization of coronary CTA analysis with calculation of CT-derived risk scores, including lesion-specific physiological metrics, will facilitate the synergism between patient care and artificial intelligence to further improve clinical outcomes in patients with CAD.”
Related CAD-RADS Content:
New CAD-RADS 2.0 reporting for coronary CTA offers patient management recommendations
Radiologists utilize novel CAD-RADS in 95% of coronary CTA reports
CAD-RADS a ‘big step in the right direction’ toward improving outcomes for acute chest pain
Continued variation in radiology tech reports poses threat to readability