Photo Gallery: ACC 2022 in pictures
This is a photo gallery of images from the 2022 American College of Cardiology (ACC) meeting. It includes new technologies and sessions from the event. This was the first in-person ACC meeting since 2019, because of the COVID pandemic.
Links to all the ACC 2022 late-breaking clinical trials
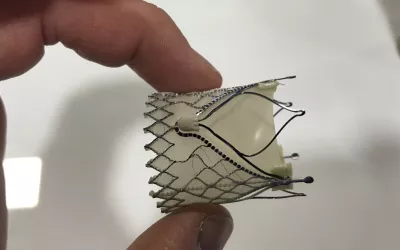
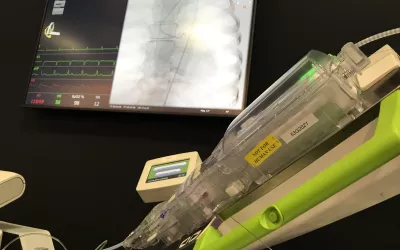
A closeup view of the JenaValve transcatheter aortic valve replacement (TAVR) device on display for the first time at ACC. It has European CE mark and it is now involved in a FDA IDE trial. It is designed to be used in patients without heavily calcified valve leaflets or annulus. It has 3 radiopaque markers to orientate it with the three valve cusps. It also has wire extensions that the native leaflets slide into and are clipped to in order to help anchor the self-expanding valve in the absence of calcium.
ACC President Dipti Itchhaporia, MD, opened up the ACC22 meeting with a message of support for fellow cardiologists and clinicians suffering in Ukraine because of the Russian invasion. ACC was among the cardiology societies to issue statements of support of Ukraine. It included thanks to the Ukrainian healthcare workers who are literally on the front lines and continuing to provide care to patients from bomb shelters and basements of their hospitals. Read more - https://www.cardiovascularbusiness.com/topics/patient-care/we-help-everyone-who-needs-it-heart-hospital-ukraine-treating-wounded-civilians
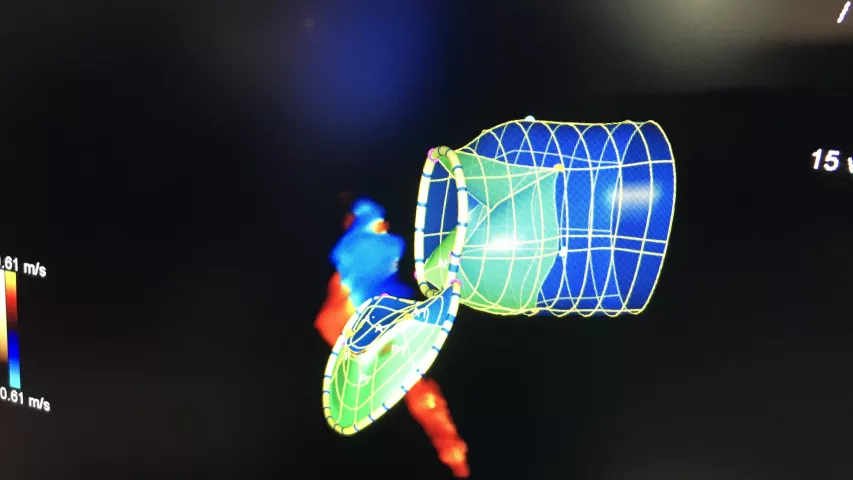
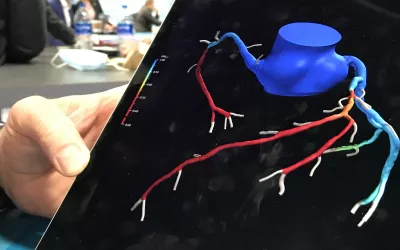
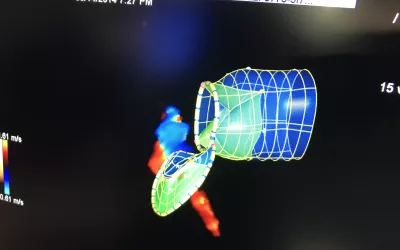
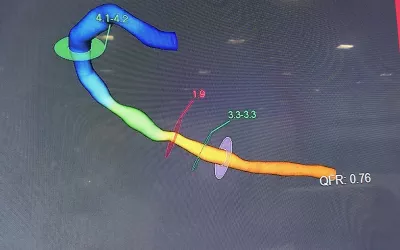
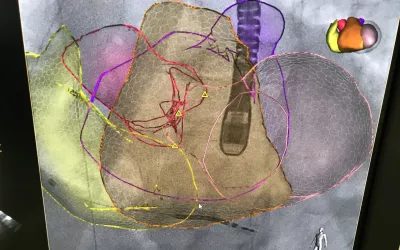
An example of a HeartFlow FFR-CT 3D rendering of a patient's coronary tree from their cardiac CT scan. A virtual, non-invasive fractional flow reserve (FFR) ratio is calculated using AI and computational fluid dynamics, rather than the current standard of care using an invasive pressure wire in the cath lab. The color codes show areas of dropping hemodynamic flow, with red areas being below acceptable levels, where the patient is experiencing ischemia. Interventional cardiologists can use the 3D rendering to plan PCI procedures.
This is the Medtronic Arctic Front cryoablation catheter used for pulmonary vein isolation (PVI) to treat arrhythmias in the EP lab. It was on display in the vendor's booth at ACC.22. This technology has been used as a replacement for point-to-point ablation catheters because it greatly speeds procedure time and creates a better ablation scar to eliminate spaces between points where errant electrical signals can still make it through and continue to cause problems for the patient or require a second ablation.
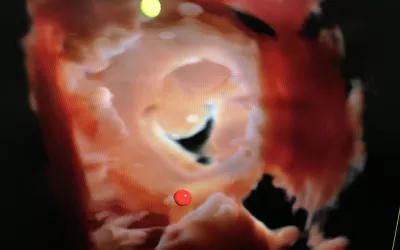
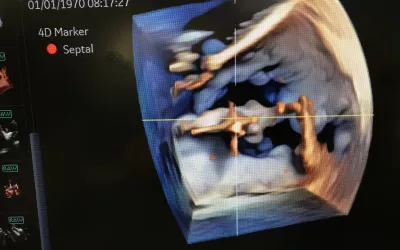
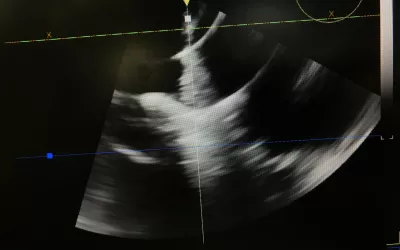
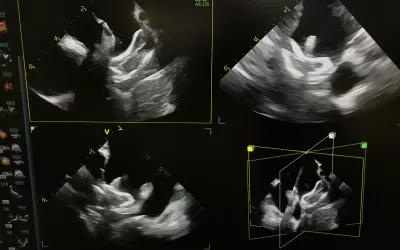
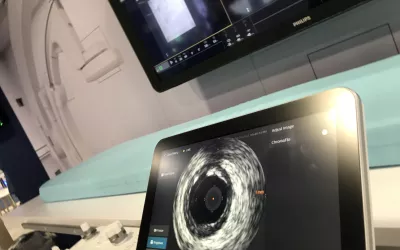
The mitral valve visualized by a GE NuVision 4D intra-cardiac echo (ICE) catheter a life-like surgical rendering technology on the Vivid E95 cardiac ultrasound system. The catheter was co-developed with Biosense Webster to perform EP procedures. It also can be used in place of TEE in structural heart procedures to eliminate the need for an interventional echocardiography.
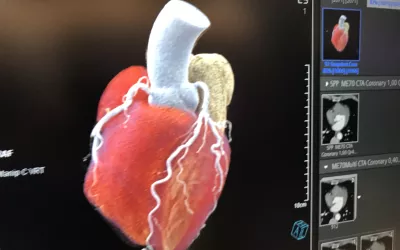
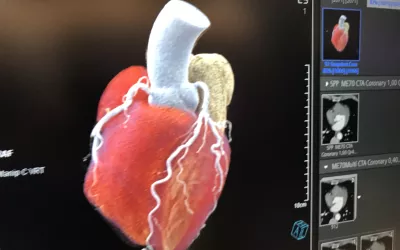
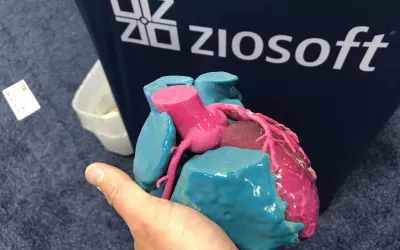
A 3D rendering of a patient's heart from a photon counting CT system in the Siemens booth. The vendor became the first to commercialize a photon-counting CT scanner in 2021, with the approval of the Naeotom Alpha. It can reduce radiation dose, produce clearer images and bins photos by energy to create spectral imaging capabilities on all scans.
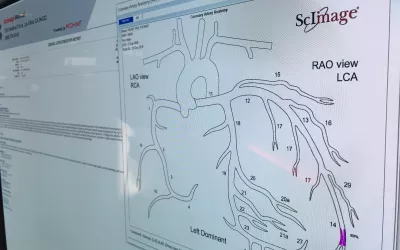
A pop-up interventional cardiology coronary tree diagram that can be annotated with stents, areas of obstructive lesions and measurements that is part of the cath reporting system in the ScImage cardiovascular information system (CVIS). Some vendors offers systems like this that will auto complete sections of the cath report based on the information entered during the procedure and from annotations on the coronary tree. This can help speed report completion.
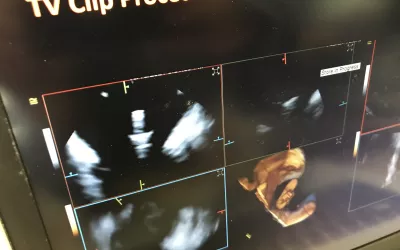
A MitraClip transcatheter mitral valve repair device visualized by a GE NuVision 4D intra-cardiac echo (ICE) catheter. The catheter was co-developed with Biosense Webster to perform EP procedures. It also can be used in place of TEE in structural heart procedures to eliminate the need for an interventional echocardiography.
ACC hosted a session that included four of the former female presidents of ACC to speak, and there was a line of attendees to speak with them on various issues and to get selfies afterwards. Left is Athena Poppas, MD, and right is Mary Norine Walsh, MD, both past ACC presidents. Watch the session on YouTube at https://www.youtube.com/watch?v=UAmcho3N9Cw
The vaccination verification station at the main entrance into the Washington Convention Center. Stickers were issues after the check that were placed on the attendees badeg to show their vaccination status was verified. This was the first time ACC held an in-person conference since 2019 because of the COVID-19 pandemic. As part of its precautions against the virus to keep the event safe, mandatory proof of COVID vaccinations had to be shown and masks were required throughout the event.
The Corindus CorPath robotic system to help guide percutaneous coronary interventions (PCI) in the cath lab. The company was purchased by Siemens Healthineers a couple years ago and the system was displayed in their booth. It allows operators to sit down in a lead-lined booth without the need for lead aprons to control joysticks, similar to a video game, to guide catheters and devices through coronary or peripheral vessels. The system can help greatly reduce operator radiation exposure from the angiography system and help prevent back pain and orthopedic issues common among interventionalists.
Example of mitral valve regurgitation on Siemens' eSie Valves echocardiography analysis software. The system can automatically render the valve to show this view of the valve and the left ventricular outflow tract (LVOT), which is necessary for assessing patients for both surgical and transcatheter valve replacements.
This is a wearable defibrillator vest for patients at risk of sudden cardiac arrest who may not need a permanent implantable cardioverter defibrillator (ICD), or who are waiting to get one. The Kestra Medical Technologies vest is the second wearable defibrillator on the market, in addition to the Zoll vest. The Kestra vest used feedback from doctors to develop vests specific to men and women for better comfort and fit. It has built-in 6-lead ECG sensors sewn into the vest that make contact directly with the patient's skin. The vendor said this lowers the amount of noise that can lead to potential false alarms. The Kestra vest gained FDA clearance in July 2021.
The Kardiogenics wearable cardiac monitor patch is able to transfer all its data directly into an EMR in a real-time feed. It it is meant for use in the ICU to eliminate wire leads, or for home monitoring. It uses Bluetooth data connectivity and can interface with an iPad for home monitoring or for use in rounds. The device is submitted for FDA review.
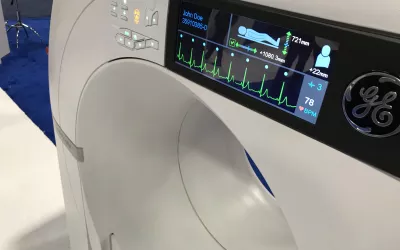
The GE/Arineta Cardiographe dedicated cardiac CT scanner in the GE booth at ACC. This small footprint system was designed to produce the best cardiac imaging possible. The small size was meant for use in small office spaces and out-patient clinics. With the new 2021 chest pain evaluation guidelines, cardiac CT was elevated to a Class 1a indication, so there was a lot of interest in this system.
TriClip device visualized using Siemens' new 4D intra-cardiac echo (ICE) catheter. The Acuson AcuNav Volume ICE catheter can help guide not only EP procedures, but also structural heart procedures for tricuspid and mitral TEER and LAA occlusion. The use of ICE can help reduce the number of people needed for a procedure, since the operator is the person guiding the ICE catheter.
TriClip device visualized using Siemens' new 4D intra-cardiac echo (ICE) catheter. The Acuson AcuNav Volume ICE catheter can help guide not only EP procedures, but also structural heart procedures for tricuspid and mitral TEER and LAA occlusion. The use of ICE can help reduce the number of people needed for a procedure, since the operator is the person guiding the ICE catheter.
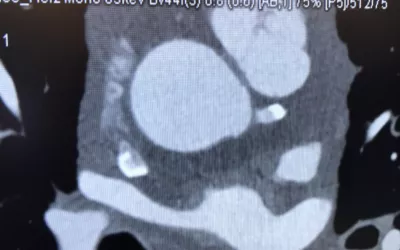
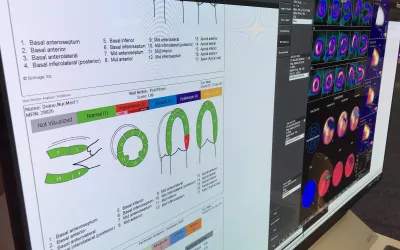
Example case of photon-counting cardiac CT shown by Siemens at it booth today at the American College of Cardiology (ACC) 2022 meeting. The Naeotom Alpha system gained FDA approval in 2021 and is the first photon-counting CT scanner commercially approved. The technology enables all scans to be multi-energy spectral scans because photons of different energies are binned so different energies renderings can be shown. It also allows removal of specific elements, so calcium or metal implants can be removed or compensated for to eliminate blooming and streaking artifacts. This also allows evaluation of a coronary lumen to visualize plaques and restenosis inside stents or in heavily calcified vessels.
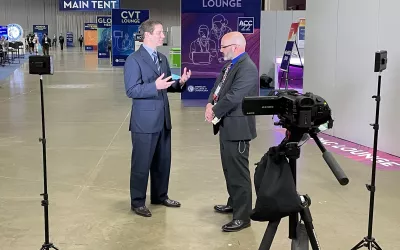
Sean Pokorney, MD, director of the arrhythmia core lab Duke Clinical Research Institute, spoke with Cardiovascular Business Digital Editor Dave Fornell on a 1 million patient late breaker on EP device lead extraction in cases of infection. The study looked at the infection rate of pacemakers and ICDs more than one year after implant. The results clearly showed antibiotics are not effective alone after device explanation and that leads also need to be removed or else there is a very high mortality rate. Many EPs shy away from lead extraction, but in the case of device infections, this study showed it should become a standard of care.
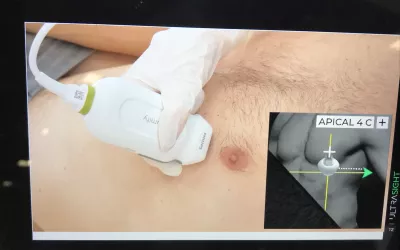
A view from a training video shown by startup artificial intelligence (AI) company UltraSight where the AI will show novice sonographers proper placement and angle of the transducer to get optimal echocardiograms. Cardiac ultrasound image quality depends largely on the operator and can be extremely variable. This AI tool is designed to compensate for this and help make all echo exams comparable across operators, regardless of their level of experience. The system uses a small picture shown here in the corner of the screen show tell the user how to position the probe and uses a color coded line to show when they are in, or approaching the correct positioning.
The wearable Cardea Solo cardiac monitor patch made by Cardiac Insight. These types of small, wearable monitors are easier to use and have been increasing used rather than traditional Holter monitors to remotely monitor patients. The device has a data capsule inside that can be removed during an in-office visit and plugged into a small reader device to download all the data into automated software that can generate a report and show sample waveforms from the patient.
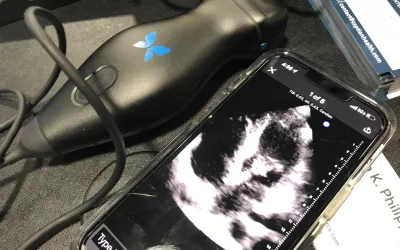
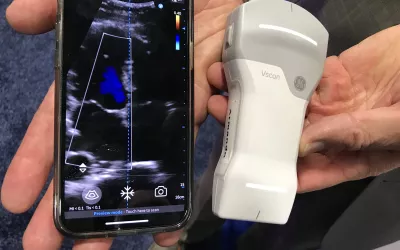
The Butterfly System point-of-care ultrasound (POCUS) system uses an app and a transducer to convert a smartphone or iPad into an ultrasound system. This was one of several POCUS systems on display at ACC.22. Butterfly has apps specific to several areas of anatomy, including vascular and cardiac. During COVID, POCUS exploded as a way to get quick looks inside COVID patients with an easy to sterilize imaging system that would not interfere with tubes, ventilators and other equipment.
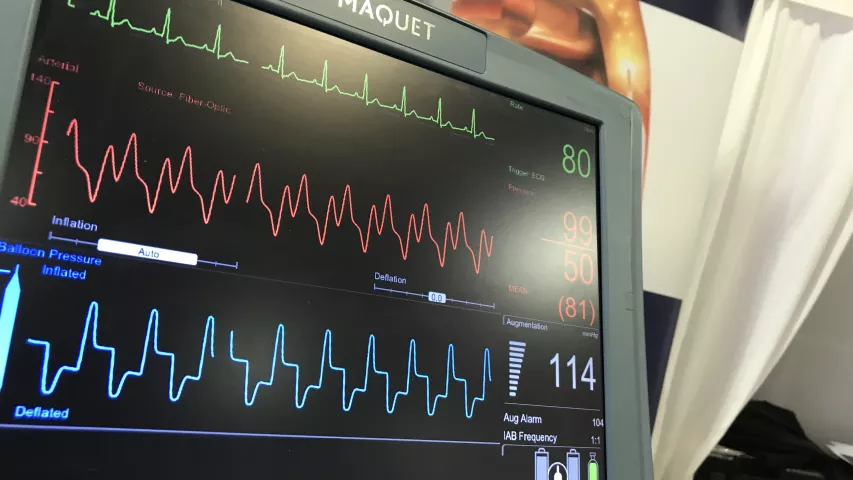
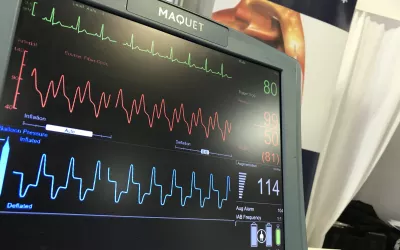
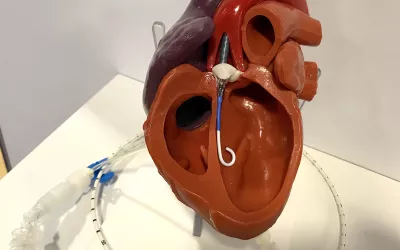
This is a model in the Abiomed booth showing the positioning of an Impella percutaneous hemodynamic support pump in the left ventricle. The pump, inserted via the femoral artery, can offer more support than an IABP. The company created its own database of studies and registry data showing improved outcomes when used in patients with severely reduced ejection fractions, in need of support during protected PCI, or in cardiogenic shock.
A wearable cardiac monitor from BioSenseTek, which offers 720 hours of battery life, connectivity within 100 meters of a base station and is waterproof so patients can shower. It is designed for use in general wards and for home monitoring. The device has European CE mark and has been submitted for FDA review.
3D intra-cardiac echo (ICE) imaging of an Amplatzer Amulet left atrial appendage (LAA) occluder implant procedure visualized using a GE Healthcare NuVision ICE catheter. Siemens and GE both showed new 4D ICE systems and said they can be used in place of TEE to help guide some structural heart procedures.
Amit Patel, MD, director, noninvasive cardiovascular imaging and director, Cardiac MRI and CT, University of Virginia, speaks during an informal GE Healthcare breakfast at ACC22 that concentrated on the use of cardiac CT under the new chest pain guidelines released in the fall of 2021. CT was raised to the top Class 1a level of evidence for use, which has spurred a lot of interest in using CTA more. The session discussion included barriers to CT use, issues with rivalry at some centers between cardiology and radiology, the fact cardiology departments with their own scanners saw significant use, and the need for more access to CT beyond hospitals in the out-patient setting.

Dave Fornell has covered healthcare for more than 17 years, with a focus in cardiology and radiology. Fornell is a 5-time winner of a Jesse H. Neal Award, the most prestigious editorial honors in the field of specialized journalism. The wins included best technical content, best use of social media and best COVID-19 coverage. Fornell was also a three-time Neal finalist for best range of work by a single author. He produces more than 100 editorial videos each year, most of them interviews with key opinion leaders in medicine. He also writes technical articles, covers key trends, conducts video hospital site visits, and is very involved with social media. E-mail: dfornell@innovatehealthcare.com