History of COVID-19 doubles long-term risk of heart attack, stroke or death
New research supported by grants from the National Institutes of Health revealed a history of COVID-19 can double a patient's risk of heart attack, stroke or death.[1] The study, published in Arteriosclerosis, Thrombosis, and Vascular Biology, found that the heightened risks can sometimes last for years after a COVID diagnosis.
The research was led by Cleveland Clinic and the University of Southern California. Anyone who had a COVID-19 infection, regardless of severity, was twice as likely to have a major cardiac event, such as heart attack, stroke or even death, for up to three years after diagnosis, the group found. The risk was significantly higher for patients hospitalized for COVID-19 and more of a determinant than a previous history of heart disease.
The researchers also found that patients with a blood type other an O (such as A, B or AB) were twice as likely to experience an adverse cardiovascular event after COVID-19 than those with an O blood type.
These findings show that the long-term risk associated with COVID-19 “continues to pose a significant public health burden” and the findings warrant further investigation, according to the authors.
Cardiology may see increasing numbers of former COVID patients in the years to come
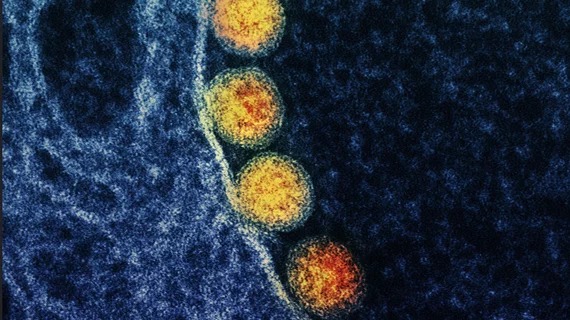
During the pandemic, there were serious concerns that the SARS-CoV-2 virus may cause an increase in future cardiovascular issues in COVID patients. This was based on the larger than expected vascular and myocardial involvement seen in many cases. What was originally thought to be long-term damage subsided in patients overtime. While concerns about heart damage and increased numbers of heart failure patients did not come to pass, this study shows evidence that cardiologists may still see increasing numbers of patients in the years to come.
“Worldwide over a billion people have already experienced COVID-19. The findings reported are not a small effect in a small subgroup,” co-senior study author Stanley Hazen, MD, PhD, chair of cardiovascular and metabolic sciences in Cleveland Clinic’s Lerner Research Institute and co-section head of preventive cardiology, said in a statement. “The results included nearly a quarter million people and point to a finding of global healthcare importance that promises to translate into a rise in cardiovascular disease globally.”
Why do COVID patients have elevated cardiovascular risks?
Researchers used U.K. Biobank data from 10,005 people who had COVID-19 and 217,730 people who did not between February and December 2020. Certain genetic variants are already linked to coronary artery disease, heart attack and COVID-19 infection, so researchers completed a genetic analysis to see if any of these known genetic variants contribute to elevated coronary artery disease risk after COVID-19. They found none of the known genetic variants were drivers of the enhanced cardiovascular events observed post COVID-19 infection. Instead, the data highlighted an association between elevated risk and blood type.
Previous research has shown that people who have A, B or AB blood types were also more susceptible to contracting COVID-19, the researchers said.
“These findings reveal while it’s an upper respiratory tract infection, COVID-19 has a variety of health implications and underscores that we should consider history of prior COVID-19 infection when formulating cardiovascular disease preventive plans and goals,” Hazen said. “The association uncovered by our research indicates a potential interaction between the virus and the piece of our genetic code that determines blood type and signals the need for further investigation.”
“Given our collective observations and that 60% of the world's population have these non-O blood types, our study raises important questions about whether more aggressive cardiovascular risk reduction efforts should be considered, possibly by taking into consideration an individual's genetic makeup," explained Hooman Allayee, PhD, of USC’s Keck School of Medicine, who was co-senior author of the paper.