Incidental breast calcifications on mammograms linked to much higher risk of cardiovascular disease
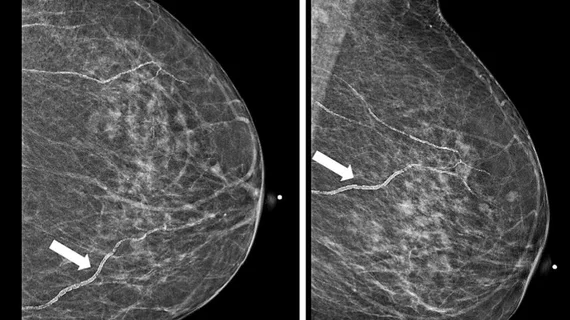
Breast arterial calcifications (BACs) identified on screening mammograms may help identify women who face a heightened risk of developing cardiovascular disease (CVD), according to a new analysis published in Clinical Imaging.[1]
“Societies such as the Canadian Society for Breast Imaging and Society for Cardiovascular Computed Tomography have recommended routine reporting of BAC when incidentally found,” wrote first author Shadi Azam, PhD, a postdoctoral associate with Weill Cornell Medicine in New York City, and colleagues. “However, there remain questions about its clinical utility and management of women who have BAC identified on screening mammography. Considering that approximately 40 million mammograms are conducted every year in the United States, understanding the pathophysiology of BAC and its relationship to cardiovascular risk factors could provide a gender-specific approach to identify women who are at a higher risk of cardiovascular disease.”
Azam et al. explored data from 215 women between the ages of 40 and 78 years old who underwent screening mammography and cardiac CT angiography (CCTA) within a two-year period. All patients received care from 2007 to 2017.
Overall, BACs were seen on the mammograms of 18% of women evaluated for this analysis. These patients presented with a higher mean BMI, a greater mean systolic blood pressure and a greater mean diastolic blood pressure than patients with no BACs. The diabetes rate was also much higher—23.7% vs. 10.2%—among patients with a BAC on screening mammography than patients without a BAC.
After adjusting for age, patients with hypertension, systolic blood pressure ≥ 130 mmHg and diastolic blood pressure ≥ 80 mmHg all had greater odds of presenting with a BAC. These findings were more likely among women with a history of childbirth, especially if she gave birth to her first child at 28-years-old or younger.
CCTA results were used to evaluate each patient for the presence of coronary arterial calcifications (CACs) so that researchers could establish relationships between BACs, CACs and a patient’s 10-year risk of atherosclerotic cardiovascular disease (ASCVD).
When no BAC or CAC were present, the 10-year ASCVD risk was 4.4%. When a BAC was present, that risk increased to 8.8%. Finally, when both BACs and CACs were present, that 10-year ASCVD risk climbed to 13.3%.
“Our results suggested a positive and significant association between being parous, having a higher number of children, giving birth at a young age, and increased likelihood of BAC,” the authors wrote. “Furthermore, we observed that the estimated risk of developing ASCVD over a 10-year period was at its lowest when neither BAC nor CAC were present, while the highest risk was found in cases where both BAC and CAC were present. The results of this study provide support for the notion that BAC detected on a routine mammogram may aid in identifying women who may have an elevated risk of developing cardiovascular disease in the future, without incurring any additional expenses or exposure to radiation.”
Additional research is still necessary, the group concluded. These studies should include larger patient cohorts and longer follow-up periods.
Click here to read the full analysis in Clinical Imaging.