Researchers receive $11.2M to study how the heart recovers from significant damage
The National Heart, Lung, and Blood Institute—part of the National Institutes of Health—has awarded an $11.2 million grant to researchers who will investigate, among other things, the possibility of restoring dead heart tissue after a myocardial infarction.
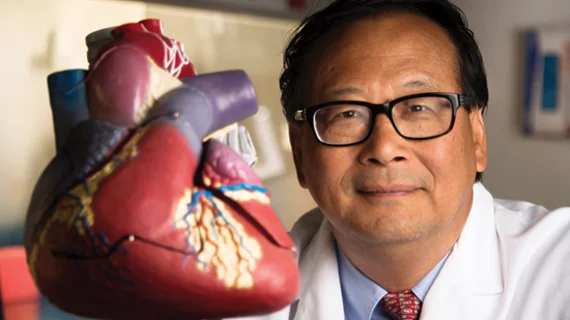
The grant will fund three related projects that each build on a recent discovery by Jianyi “Jay” Zheng, MD, PhD, and colleagues, that neonatal pigs can remuscularize dead heart tissue through cardiomyocyte proliferation. Normally, dead tissue will eventually be replaced by scar tissue, which can strain remaining heart muscle and may eventually contribute to heart failure.
“Recent preliminary studies from our laboratories using neonatal pigs have shown that, when a myocardial infarction is induced on postnatal day 1, or P1, cardiomyocytes reenter the cell cycle, proliferate and completely restore cardiac function with little scarring,” Zhang, chair of the University of Alabama at Birmingham’s Department of Biomedical Engineering, said in a statement.
Zhang will lead the first project, which aims to identify cardiomyocyte cell-cycle regulators and learn how to target them in a way that will cause cardiomyocytes to re-enter the cell cycle and proliferate. Additionally, researchers will use stem cells to generate novel “muscle patches” with activated cell-cycle regulators and layers of other cardiac cells. Then—using what they discover about targeting regulators as well as the muscle patches—the researchers will attempt to remuscularize adult pigs’ hearts after a heart attack.
“The findings from the large-mammal cardiac muscle regeneration will have unprecedented clinically relevant dimensions,” the statement notes.
In the second NIH-funded project, Daniel J. Garry, MD, PhD, of the University of Minnesota Medical School, will lead researchers in investigating whether they can promote cardiomyocyte proliferation in adult mice and pigs by using certain effectors of the Sonic Hedgehog developmental pathway.
In the third project, Hesham Sadek, MD, PhD, of the University of Texas Southwestern Medical Center, “looks at the intriguing hypothesis that selective utilization of proline metabolism promotes the survival of heart ventricular myocytes and proliferation under conditions of low oxygen.”