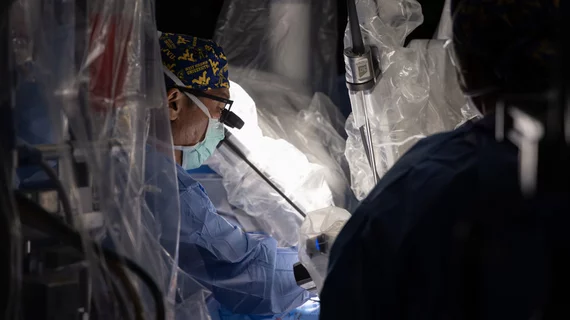
Heart surgeons perform world’s first combined robotic AVR and CABG
Heart surgeons with the WVU Heart and Vascular Institute have made a bit of history, performing the world’s first combined robotic aortic valve replacement (AVR) and coronary artery bypass grafting (CABG) procedure—all through one small incision. Patients requiring these procedures typically undergo open-heart surgery.
The patient in question, 73-year-old Poppy McGee, presented with a history of stroke, brain surgery and ongoing weight loss. She was referred to Vinay Badhwar, MD, executive chair of the WVU Heart and Vascular Institute and chair of WVU’s department of cardiovascular and thoracic surgery, who initially recommended open-heart surgery. However, when McGee and her family heard that the odds of dying exceeded 10%, they inquired about less invasive treatment options.
Badhwar, a known pioneer of robotic aortic valve replacement (RAVR) and other robotic surgical techniques, said his team had developed a new technique for combining AVR and CABG—but it had not yet been tested on a patient. After a long discussion with McGee and her family about the risks, she agreed to the new-look surgical treatment.
The combined surgery occurred on Oct. 31, 2024. Both the AVR and the CABG were performed using the same small incision on the far right of McGee’s chest. The surgery was a success, and a detailed account is expected to publish in The Annals of Thoracic Surgery.
“While we are still in the early days of this latest innovation, the ability to perform valve surgery and coronary artery bypass surgery fully robotically through a single incision has the potential to open up a new era of robotic heart surgery,” Badhwar said in a prepared statement announcing the procedure. “We must always keep quality outcomes at the forefront of all innovation. However, if surgeons adopt and gain experience with techniques such as this one, they will tackle this last frontier that previously limited a robotic approach. One day in the near future, this may serve as a platform to perform nearly all types of heart surgery.”
“We are so thankful for Dr. Badhwar and the team at the WVU Heart and Vascular Institute developing this robotic procedure to help my mother recover so well,” added Mollie Wilcosky, McGee’s daughter. “She is getting stronger every day, and we were able to enjoy a nice Thanksgiving with her at home.”
A sign of things to come?
In the same statement, Goya Raikar, MD, a member of Badhwar’s robotics team and an assistant professor a WVU, highlighted the progress this successful procedure represents for their work on advancing robotic surgical techniques.
“Until now, the main exclusion for us to perform a robotic approach has been the coexistence of valve and coronary artery disease,” he said. “Building on our experience with robotic aortic valve surgery, this new approach may help us extend robotic surgery options to many more patients.”