Society of Thoracic Surgeons shares 2 new risk calculators for guiding treatment decisions
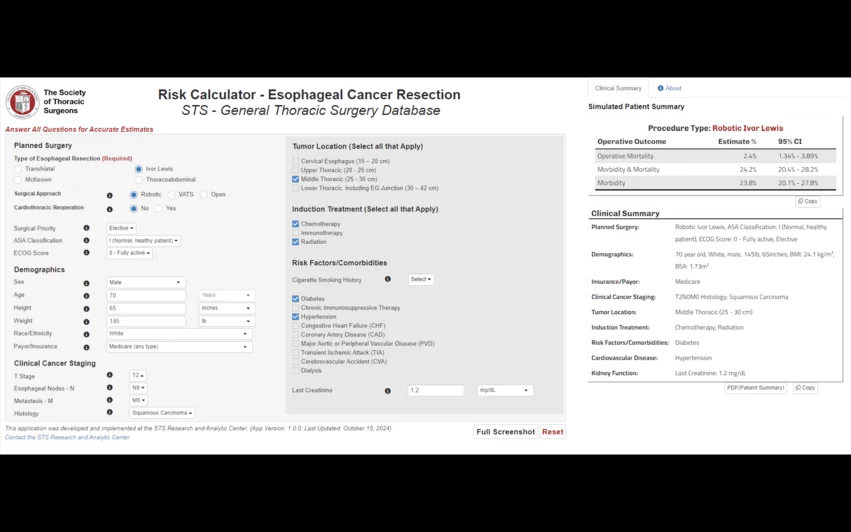
The Society of Thoracic Surgeons (STS) has released two new risk calculators designed to help care teams and their patients make the most appropriate treatment decisions possible. While one is focused on esophagectomy, the other addresses pulmonary resection.
Both new calculators were developed using updated data from the STS General Thoracic Surgery Database, a resource estimated to include detailed information from nearly 10 million cardiothoracic surgery procedures.
Surgeons have been turning to STS rick calculators for years to estimate the potential outcomes of different procedures based on specific patient characteristics. In fact, the organization’s mortality scores are often used in cardiothoracic research to help categorize patients into different risk groups. These newest risk calculators are mobile-friendly, ensuring care teams can use them whenever necessary.
A closer look at new online resources
The risk calculator focused on esophagectomy for cancer was developed with data from more than 18,000 patients who underwent treatment from 2015 to 2022. It covers new risk factors not seen in previous models, including preoperative cancer staging and body surface area.
“The esophagectomy for cancer risk calculator represents a significant advancement in personalized care for thoracic surgery patients,” STS President Jennifer C. Romano, MD, MS, said in a statement. “Informed by a more diverse patient cohort, and using preoperative variables, the tool provides surgeons and patients with a comprehensive and informed view of predicted outcomes.”
The risk calculator focused on pulmonary resection for lung cancer, meanwhile, is based on data from nearly 141,000 patients who underwent treatment from 2015 to 2022. It was made with more modern surgical techniques, including robot-assisted procedures, in mind.
“The new risk calculator for pulmonary resection of lung cancer offers superior performance and applicability, especially for high-risk patients,” Romano said. “It serves as a valuable tool for both clinical decision-making and improving patient outcomes.”
The two new risk calculators are available here.