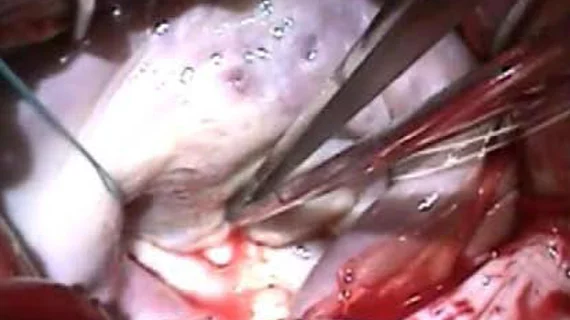
An updated look at surgically repairing the mitral valve due to mitral regurgitation
Surgically repairing the mitral valve (MV) due to primary mitral regurgitation (MR) is associated with an incredibly low risk of death, according to a new analysis published in both The Annals of Thoracic Surgery and the Journal of the American College of Cardiology.[1,2]
The study, a collaboration between cardiologists and cardiothoracic surgeons, was designed to gain a better understanding of the outcomes and risks associated with surgical MV repair. The researchers explored data from more than 50,000 patients who underwent MV repair from July 2014 to June 2020 throughout the United States. Patients included in the study were treated at 881 different hospitals, highlighting the variety of individuals the team was able to identify and examine.
Overall, mortality was seen in 1.16% of patients. Mortality and/or morbidity was seen in 8.88% of patients, and 6.36% of patients required a change from MV repair to MV replacement. Mortality was more likely among older patients, women, patients presenting with more comorbidities, and patients with a severe tricuspid regurgitation.
In addition, patient mortality was much less likely at hospitals where surgical MV repairs were performed more frequently. Most hospitals reported no cases, or just one case, of operative death. And 81% of surgeons had no operative deaths throughout the entire length of the analysis.
The authors used these findings to craft updated mortality risk models for patients being considered for surgical MV repair due to primary MR. Their algorithm determined that the predicted risk of operative mortality (PROM) was less than 3% for 97% of patients. When only focusing on patients who underwent isolated MV repair with no concomitant procedures, meanwhile, the PROM was less than 1.5% for 97% of patients.
“The mortality risk model had excellent discrimination and calibration and confirmed very low mortality risk for isolated mitral valve repair,” Robert Habib, PhD, a statistician with the Society of Thoracic Surgeons (STS), said in a prepared statement. “For the vast majority of patients, the risk of death related to this procedure was less than 1%.”
What about transcatheter mitral valve interventions?
The study’s authors emphasized that this research may change the perspective of some clinicians who have been impressed by the rise of transcatheter edge-to-edge repair (TEER) in recent years.
“Past perceptions of the risk of surgery and repair rates based on older risk models may have influenced the design of two clinical trials to explore transcatheter therapy in lower risk older individuals,” lead author Vinay Badhwar, MD, a professor with West Virginia University, said in the same prepared statement. “The finding of 90% successful surgical repair with less than 1% mortality now achieved in the United States sets the outcome bar fairly high when considering alternative therapies to surgery. We hope this information will help physicians and patients make more informed decisions regarding treatment, as well as to inform the optimal design of future trials in the field.”