Bring on the veggie burgers? Replacing meat with plant-based alternatives may boost heart health
Grocery stores have started selling more and more plant-based meat alternatives (PBMAs) in recent years, allowing families to dine on dinner staples such as burgers, hot dogs and chicken fingers without consuming a single bite of meat. PBMAs aren’t necessarily the healthiest thing a person can eat—recommendations from the American Heart Association and other groups always emphasize that plant-based diets should still focus on fruits and vegetables over meat alternatives—but they may still be better for the heart than the meat they were designed to replace.
First author Matthew Nagra, ND, a nutrition specialist at the University of British Columbia, and colleagues explored the available evidence on PBMAs, hoping to learn as much as possible about this growing trend. The team shared its findings in a new analysis published in the Canadian Journal of Cardiology.[1]
Nagra et al. noted that is easy to look down on these meat alternatives due to the fact that they are typically ultra-processed foods (UPFs) that may contain various flavor enhancers or food coloring. Research has shown that UPFs can increase a person’s risk of cardiovascular disease (CVD), leading many nutritionists to dismiss PBMAs without a second thought, but the authors emphasized that not all UPFs have the same impact on health.
“For example, sugar-sweetened beverages and processed meat have been associated with an increased risk of CVD, but whole wheat bread and whole grain cereal have been associated with a reduced risk,” they wrote. “Whether PBMAs pose a health concern similar to some other UPFs, if at all, is a nutrition question without a clear answer.”
How are plant-based meats made? It depends
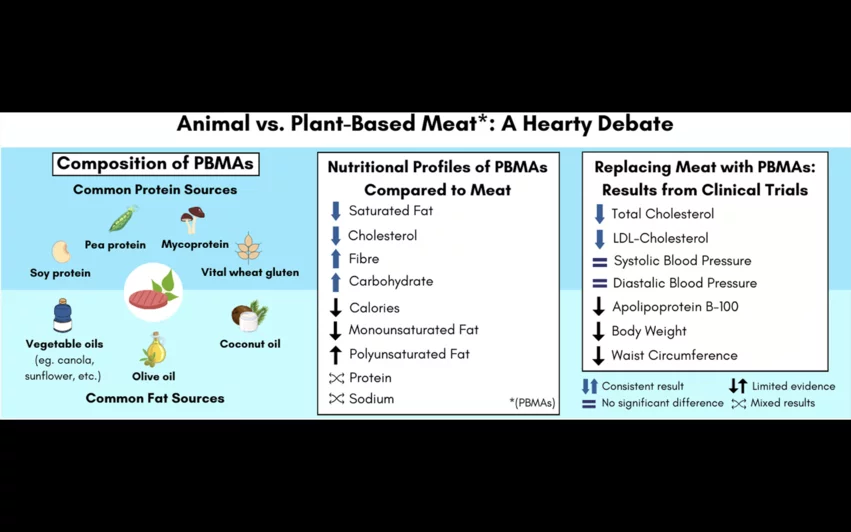
One challenge when reviewing this topic, the authors added, is that the ingredients found in PBMA can “differ substantially,” even when looking at similar products that sit right beside each other on the grocery store shelves. Most PBMAs are made with soy, pea, wheat or mushrooms, but many brands seem to have their own formulas.
The differences carry over to nutritional value. For example, the authors wrote, a plant-based burger from Impossible Foods contains 6 g of saturated fatty acid, 370 mg of sodium and 5 g of fiber. A plant-based burger sold by the Dr. Praeger’s brand, however, contains 1 g of saturated fatty acid, 530 mg of sodium and 3 g of fiber.
“Despite the variability among PBMAs, according to a 2022 review, several analyses conducted in different international markets have suggested that they generally have a more favorable nutrient profile for reducing the risk of CVD compared with meat while also being more environmentally sustainable protein sources,” the authors wrote.
Reviewing the evidence
Nagra and colleagues tracked down years of research about PBMAs, focusing much of their on six randomized controlled trials that put different diets to the test.
One of those studies, SWAP-MEAT, explored the impact of eating pea protein-based PBMAs manufactured by Beyond Meat instead of grass-fed meat.[2] The 16-week trial asked participants to eat two or more servings of either PBMAs or meat per day for eight weeks before crossing over and switching to the other option for another eight weeks. Consuming PBMAs was associated with reductions in body weight and LDL-C levels, with no significant differences in blood pressure, inflammation biomarkers, fiber, sodium or protein.
A separate trial focused on red meat, white meat and plant protein led to similar results.[3]
“The available randomized controlled trials evaluating PBMAs are promising and suggest that replacing meat with PBMAs can improve CVD risk factors, including a reduction in LDL-C,” the authors wrote. “PBMAs do not seem to negatively affect other CVD risk factors such as blood pressure, despite their classification as UPFs and the high sodium content of many products. These improvements in CVD risk factors may result in a lower risk of developing CVD; however, there is a need for high-quality long-term studies evaluating CVD outcomes.”
Click here to read the full breakdown, which provides more details about each study the team evaluated.